Digestion and the Circulatory System
Digestion
Large food molecules cannot fit through cell membranes so they need to be broken down before they can be absorbed by the cells lining the intestine.
Digestive enzymes beak the bonds in macromolecules (e.g. carbohydrates, proteins, lipids) into monomers.
This is a hydrolysis reaction – it uses a water molecule to break bonds.
Monomers such as glucose, amino acids, fatty acids and glycerol are then transported into the ileum of the intestine and diffuse into the bloodstream.
Digestion and absorption of carbohydrates
Amylase breaks down starch into maltose (a disaccharide) by catalysing the hydrolysis of glycosidic bonds. It is made in the salivary glands and the pancreas. The salivary glands secrete amylase into the mouth, where starch begins to be hydrolysed. The pancreas secretes amylase into the small intestine, where remaining starch is digested.
Disaccharidases such as maltase break down disaccharides into monosaccharides in the small intestine. Some of these are attached to the epithelial cells lining the ileum and are known as membrane-bound disaccharidases.
Maltase hydrolyses maltose into two glucose molecules.
Sucrase hydrolyses sucrose into glucose and fructose.
Lactase hydrolyses lactose into glucose and galactose.
These monosaccharides are small enough to be transported across the plasma membrane of the epithelial cells lining the ileum. Glucose is absorbed by cotransport with sodium ions (a process which requires the active transport of sodium ions out of the epithelial cell). Fructose is absorbed by facilitated diffusion.
Digestion and absorption of lipids
Lipids are hydrolysed into monoglycerides (glycerol with one fatty acid still attached) and fatty acids. Lipase breaks down lipids by hydrolysing the ester bonds in the lipid.
Lipases are synthesised in the pancreas then released into the small intestine. Lipid digestion is facilitated by the production of bile salts in the liver. Bile is stored in the gall bladder then released into the small intestine, where it emulsifies large lipid droplets into smaller ones. Emulsification provides a larger surface area for lipase to act on to speed up digestion.
One the lipids are fully digested, the small lipid droplets made up of monoglycerides and fatty acids combine with the bile salts to form structures called micelles. These help to move the digested lipid towards the epithelium. Micelles are dynamic structures, continually breaking apart and reforming. When this happens, they spit out monoglycerides and fatty acids which can pass straight through the bilayer by simple diffusion (as they are lipid-soluble).
Digestion and absorption of proteins
Proteases break down proteins into amino acids by hydrolysing peptide bonds. Some proteases are made in the pancreas and released into the small intestine, while others are made in the cells lining the stomach and released into the stomach.
Endopeptidases digest polypeptides by breaking peptide bonds in the middle of the chain. This converts longer polypeptides into shorter ones. Pepsin is an endopeptidase which digests proteins in the stomach under acidic conditions.
Exopeptidases digest polypeptides by breaking peptide bonds at the ends of the chain. This releases individual amino acids which can be transported into the ileum epithelial cells. Dipeptidases are exopeptidases that hydrolyse the peptide bonds in dipeptides and are often bound to the membrane of the epithelial cells – this maintains a concentration gradient of amino acids for absorption.
Amino acids are absorbed by cotransport with sodium ions. Sodium ions are actively transported out of the epithelial cell, creating a sodium ion gradient which can be used to take both sodium ions and amino acids into the cell.
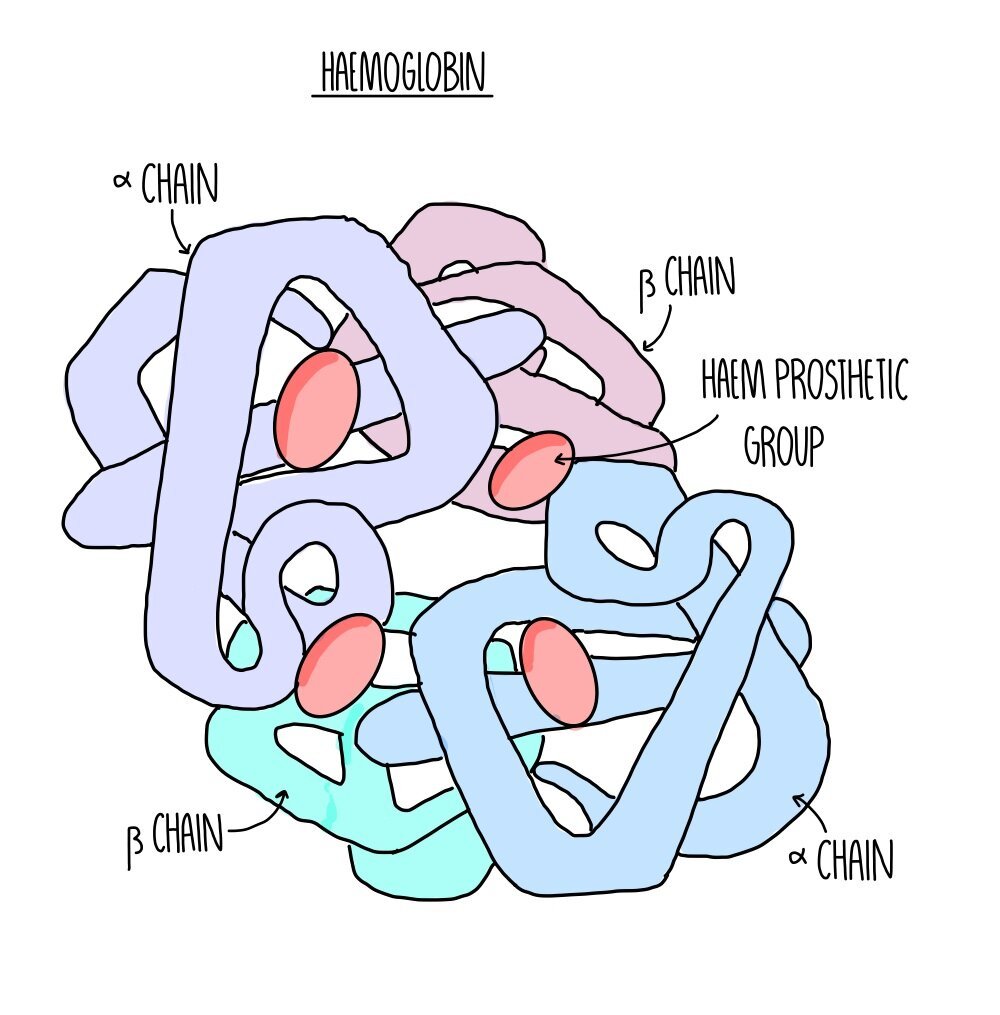
Haemoglobin
Oxygen is transported by binding to haemoglobin in red blood cells. Haemoglobin is a large, globular protein with a quaternary structure made up of four polypeptide chains. Its four subunits each possess a haem group containing an iron ion. Four oxygen molecules can bind to the four haem groups to form oxyhaemoglobin.
Haemoglobin saturation and dissociation curves
Haemoglobin has different affinities for oxygen at different oxygen concentrations (partial pressures). Affinity means how ‘sticky’ haemoglobin is – the higher it’s affinity, the stronger it binds. Haemoglobin binds to oxygen with high affinity in the lungs, where there is a high partial pressure of oxygen. Haemoglobin binds with low affinity at respiring tissues, which there is a low partial pressure of oxygen. This causes oxyhaemoglobin to deposit oxygen at the tissues so they can use it for aerobic respiration.
You can see this on a dissociation curve, which shows how saturated haemoglobin is with oxygen at different partial pressures.
The graph has a sigmoid, or S-shaped, because binding of the first oxygen molecule causes oxygen to change shape and uncover the other oxygen binding sites. This makes it easier for further oxygen molecules to bind and is known as cooperative binding. Once three oxygen molecules are bound, it is harder for the final one to bind because there is only one binding site available.
The Bohr Effect
Haemoglobin’s affinity for oxygen also changes at different concentrations of carbon dioxide. At higher partial pressures of carbon dioxide, haemoglobin has a lower affinity for oxygen, causing oxyhaemoglobin to dissociate more readily.
This is useful because tissues with high rates of respiration (so greater need for oxygen) will be producing larger amounts of carbon dioxide. This ensures that oxygen is unloaded from haemoglobin at respiring tissues.
High carbon dioxide concentration shifts the dissociation curve to the right. It is referred to as the Bohr Effect.
Dissociation curves for different organisms
Organisms that live in different environments are adapted to allow them to survive in different oxygen concentrations. Organisms that live in low-oxygen environments (e.g. waterlogged soils) have a dissociation curve that lies to the left – this means that haemoglobin is good at binding to oxygen when partial pressures are low. Organisms that are especially active (e.g. birds of prey) have a dissociation curve that lies to the right – this means that haemoglobin is good at releasing oxygen at higher partial pressures so that their cells can use it to respire.
A = organism adapted for conditions of low oxygen availability e.g. lugworm
B = organism adapted for living at high altitude where oxygen partial pressure is lower e.g. llama
C = organism adapted to living at normal partial pressures of oxygen e.g. human
D = active organisms with high rates of respiration and plenty of oxygen availability e.g. eagle
Mammals need mass transport systems
Organisms need oxygen and glucose to produce energy in aerobic respiration. Small organisms, like bacteria, can obtain these by diffusion because of the short diffusion distance. But multicellular organisms have a small surface area to volume ratio so diffusion would be too slow to reach the cells in the centre of their body, so they have mass transport systems.
Mass transport systems, such as the circulatory system in mammals, deliver oxygen and glucose to all body cells. They also remove waste products (carbon dioxide and water).
Structure of blood vessels
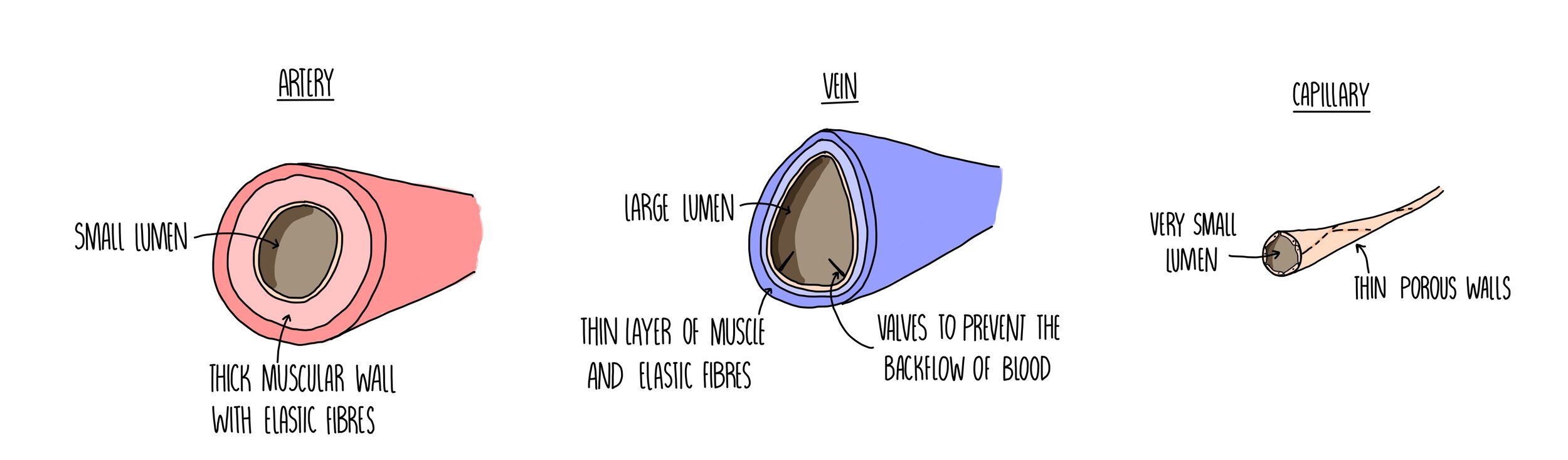
Arteries
Carry blood away from the heart to the various organs of the body.
They need to cope with the high pressure generated from the heart forcing out blood with each heartbeat. This is why they have a really thick muscular wall containing lots of elastic tissue.
The inner lining of the arteries, called the endothelium, is folded which allows the artery to expand (elastic recoil) which also helps it to withstand the high pressure.
The small lumen ensures a high pressure is maintained.
Veins
Carry blood from the organs of the body towards the heart.
Blood is flowing at a much lower pressure so veins have a large lumen and much thinner walls containing little elastic fibres or muscle tissue.
Valves prevent the slow-moving blood from flowing backwards.
The contraction of nearby body muscles helps blood to flow through veins.
Capillaries
Connect arteries and veins.
Substances move out of the blood to the body tissues - things like oxygen, glucose and mineral ions. Any waste products, such as carbon dioxide and water, will move out of the body tissues and into the capillaries.
Small holes (pores) enable the exchange of substances.
Walls are just one cell thick which reduces the diffusion distance for these substances.
There are a large number of capillaries (capillary beds) which increases the surface area available for exchange.
Tissue fluid
Tissue fluid is the fluid that bathes cells in tissues. It is made up of the substances that are small enough to move out of the capillary, such as water, oxygen, glucose and mineral ions. It also contains the waste products released from cells, like carbon dioxide, water and urea. It doesn’t contain things that are too big to be forced out of the capillary, so there are no red blood cells or large proteins.
The formation of tissue fluid takes place when smaller substances are pushed out of the capillary bed:
At the arteriole end of the capillary, hydrostatic pressure in the capillary exceeds that of the tissue fluid. This forces fluid and dissolved substances out of the capillary (down a pressure gradient) and into the spaces around the cells, forming the tissue fluid.
At the venule end of the capillary, there is less water (because it moved out of the capillary at the venule end). This means that the water potential is lower inside the capillary compared to the tissue fluid. Water moves back into the capillary by osmosis down a water potential gradient.
Excess tissue fluid drains into the lymphatic system which eventually returns the fluid back into the bloodstream.
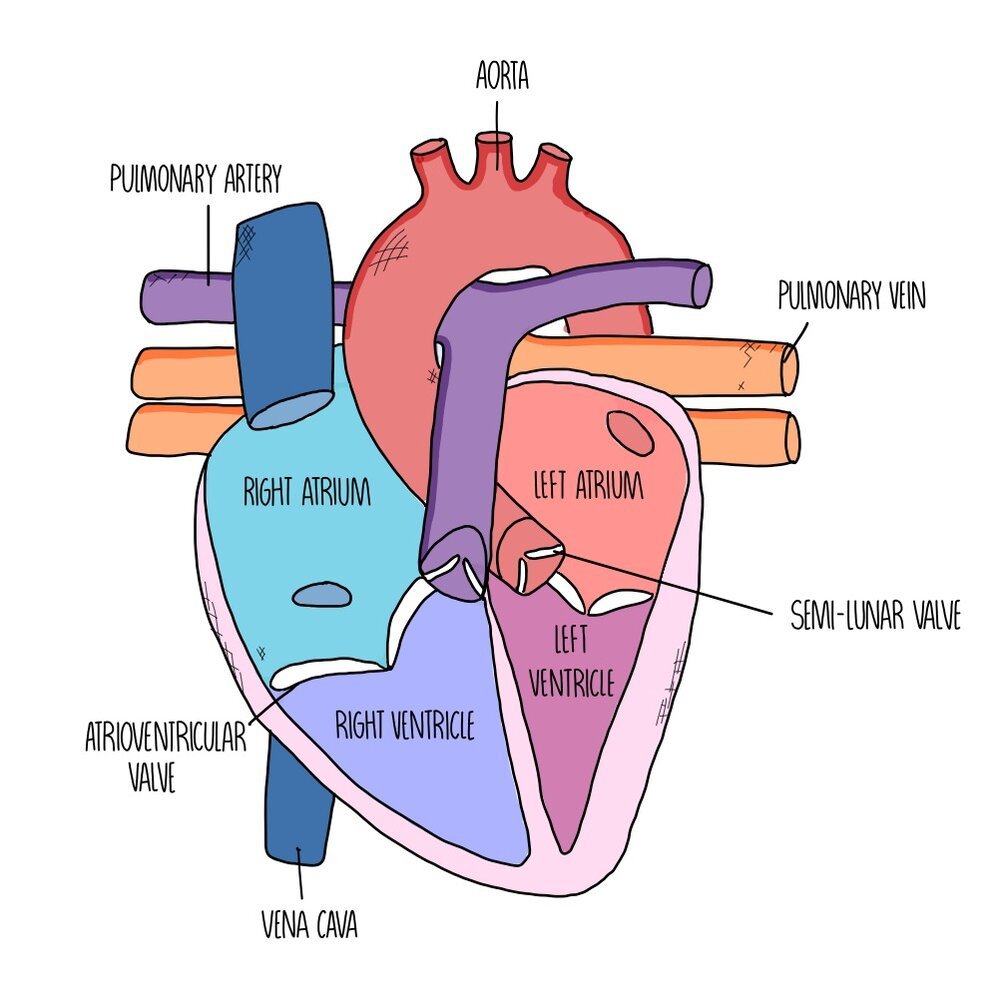
Heart structure
The heart is made up of four chambers divided into two sides. The left side of the heart has a thicker wall, as it needs to pump more strongly to deliver blood all around the body (whereas the right side just needs to send the blood to the lungs). The left side carries oxygenated blood whereas the right side carries deoxygenated blood.
The chambers at the top are called atria and these chambers receive the blood from the veins supplying the heart. Blood flows from the atria to the ventricles, which are separated from the atria by atrioventricular valves to prevent blood flowing in the opposite direction. There are another set of valves between the ventricles and the arteries which are called the semi-lunar valves as they look like little half-moons.
The main artery which takes oxygenated blood from the left side of the heart to the rest of the body is called the aorta whereas the artery which delivers deoxygenated blood between the right side of the heart and the lungs is called the pulmonary artery. The major vein which returns blood from the body to the right side of the heart is the vena cava and the vein which ferries blood from the lungs to the heart is called the pulmonary vein.
heart muscle itself also needs its own blood supply, so that it can get plenty of oxygen and glucose to keep respiring and keep pumping - these are called the coronary arteries. It’s a blockage in these coronary arteries which leads to a heart attack.
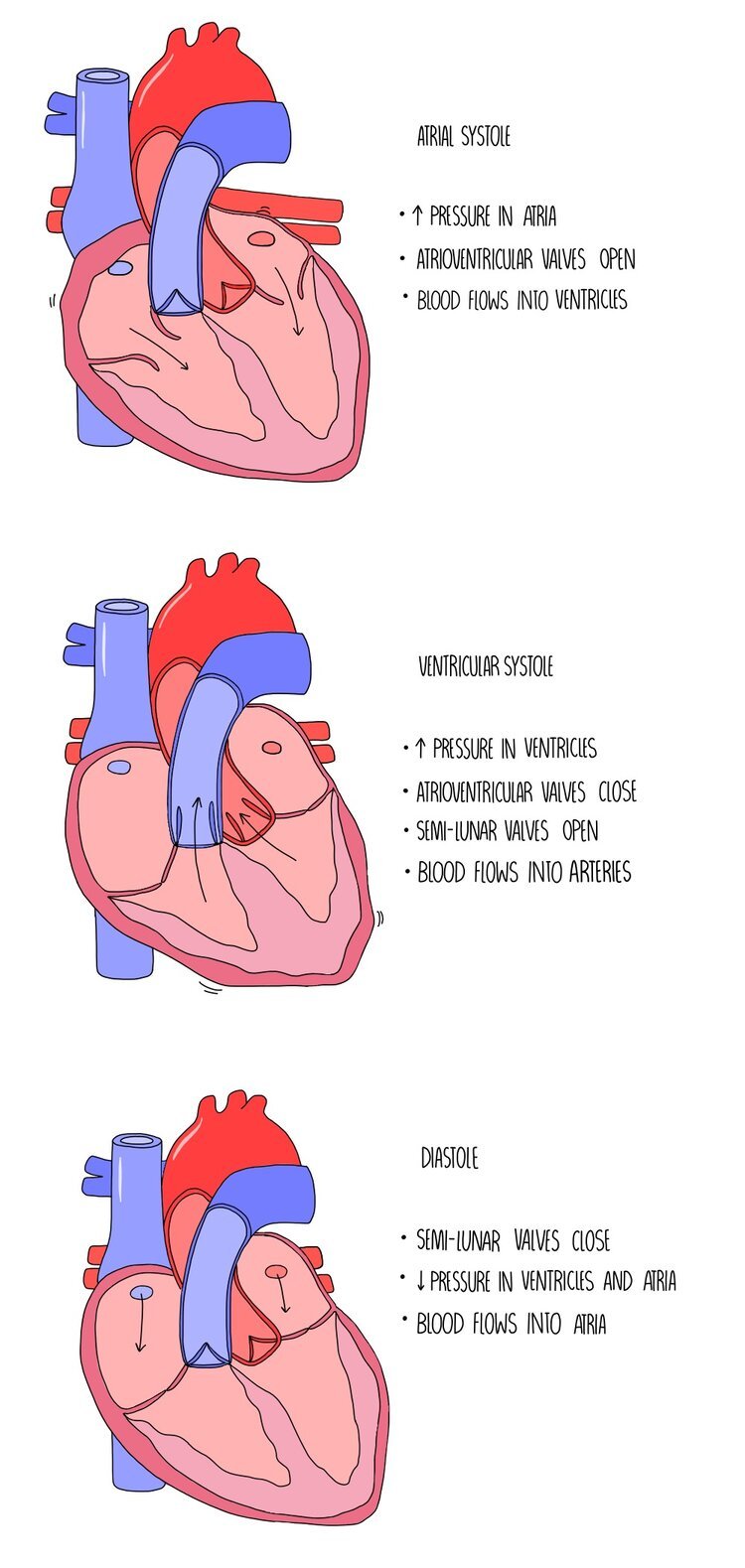
The Cardiac Cycle
The cardiac cycle is a coordinated sequence of contractions and relaxations by the heart muscle which causes blood to move from the atria, into the ventricles and then the arteries. Muscle contractions are referred to as systole and relaxation is referred to as diastole. The movement of blood through the different compartments of the heart rely on changes in volume and pressure as a result of the contraction of the heart muscle walls. It occurs in the three following stages:
1. Atrial systole
The atria contract while the ventricles relax. This decreases the volume inside the atria which increases the pressure. This increased pressure forces the atrioventricular valves open and pushes blood into the ventricles.
2. Ventricular systole
The ventricles contract while the atria are relaxed. This decreases the volume inside the ventricles which increases the pressure. The pressure is higher in the ventricles compared to the atria, which forces the atrioventricular valves closed and causes the semi-lunar valves to open. The closure of the AV valve is important because it prevents the back-flow of blood into the atria. Blood is forced out of the ventricles and into the arteries (the aorta and the pulmonary artery).
3. Diastole
Both the atria and ventricles are relaxed so the pressure is low in both chambers. Since the pressure is higher in the arteries than in the heart chambers, the semi-lunar valves are forced closed which prevents blood flowing backwards into the ventricles. Blood is returned to the heart and the atria fill with blood.
Atheroma formation
Atherosclerosis a process in which the artery lining becomes hard due to the build-up of fatty material in the artery wall. It is a problem because it can lead to the artery becoming completely blocked, cutting off blood circulation and leading to events like a heart attack or stroke. It occurs in the following stages:
The inner lining of the artery wall (the endothelium) becomes damaged due to high blood pressure (hypertension).
This triggers an inflammatory response - white blood cells (such as macrophages) move towards the site of damage and accumulate with lipids (fats) which are circulating in the blood. The accumulation of these substances underneath the artery wall leads to the formation of fatty streaks in the endothelium.
The fatty streaks develop into an atheroma, causing the lumen of the artery to become narrower and restricting blood flow. This causes blood pressure to increase further.
The hardening of arteries, caused by the development of atheromas, is referred to as atherosclerosis.
Cardiovascular disease
The formation of an atheroma in an artery causes partial blockage of an artery. If the atheroma ruptures, it can trigger a blood clot to form which may completely prevent blood flow. The stages of this process occur as follows:
The atheroma ruptures and bursts through the endothelium of the artery, damaging the artery wall.
This triggers blood clotting (thrombosis) at the site of damage.
The blood clot can cause a complete blockage within the artery.
This prevents blood flow in the artery which means that oxygen isn’t delivered to the tissues downstream of the artery.
The cells within the tissue cannot carry out aerobic respiration and will start to die.
f the blockage occurs in a coronary artery (the vessels that supply the heart), blood flow to the cardiac muscle is cut off and the tissue stops respiring. This leads to myocardial infarction (heart attack) which causes chest pains, shortness of breath and is often fatal.
Aneurysm
The formation of an atheroma increases the risk of aneurysm, a process in which the artery forms a balloon-like swelling. Plaques weaken and narrow arteries, causing blood pressure to rise. High pressures can push on through the artery lining to the outer elastic layers, causing the artery to balloon out and form an aneurysm. The aneurysm may burst and bleed out (a haemorrhage).
Risk factors for CVD
Things which increase our risk of developing cardiovascular disease can be grouped into lifestyle factors (things which result from our behaviour and are under our control) and non-lifestyle factors (things that we were born with and cannot control). Some of these factors are interlinked - for example, the genes you have may mean that you are more susceptible to high blood pressure, which is also affected by your diet.
Lifestyle factors
Smoking
The nicotine in cigarette smoke makes platelets stickier, increasing the chance of a blood clot forming which could lead to blockage in the arteries.
Carbon monoxide in cigarette smoke binds to haemoglobin in red blood cells, reducing the amount of oxygen being transported in the blood. This means the heart has to pump faster to get the same amount of oxygen delivery, which increases blood pressure.
Smoking also reduces levels of antioxidants in the blood. Antioxidants are molecules in our body which can protect the arteries from damage. The reduced levels of antioxidants in smokers can increase the likelihood of endothelial damage and atheroma formation.
High blood pressure
High blood pressure puts more strain on the artery walls and means they are more likely to suffer damage. This leads to the process of atherosclerosis which in turn can lead to blood clotting and cardiovascular disease.
A diet high in salt, high alcohol consumption, inactivity and stress can increase blood pressure.
Diet
A diet high in saturated fats and low in unsaturated fats can increase the risk of CVD. Consumption of saturated fats increases blood cholesterol levels which increase the likelihood of atheroma formation.
A diet high in salt can increase the risk of CVD by increasing blood pressure.
Lack of exercise
A sedentary lifestyle can increase the chances of CVD by increasing blood pressure.
Non-lifestyle factors
Age
The risk of CVD increases with age (heart attacks are much more uncommon in people under the age of 40).
This is because the fatty deposits which accumulate in our arteries build up over time.
Genetics
Some people possess alleles which increase cholesterol production or make them more susceptible to high blood pressure.
Likewise, other people can inherit beneficial alleles which will reduce their risk of CVD by dampening down cholesterol production or giving them slightly lower blood pressure.
Gender
Men are at a much greater risk of developing CVD than women due to lower oestrogen levels.
Oestrogen increases the levels of ‘good’ cholesterol (HDLs) which removes the amount of cholesterol circulating in the blood. This reduces the risk of atheroma formation.