Homeostasis
Homeostasis
Homeostasis is the maintenance of a constant internal environment. Things like our temperature, blood pH and blood glucose concentration needs to stay relatively stable in order to keep our cells functioning effectively. If internal conditions such as temperature or pH within our bodies don’t remain within certain limits, then enzymes will become denatured. Fluctuations in temperature result in hydrogen bonds breaking within the enzyme’s structure whereas changes in pH cause hydrogen and ionic bonds to break. The enzyme loses the shape of its active site and can no longer catalyse important biological reactions, such as respiration or DNA replication.
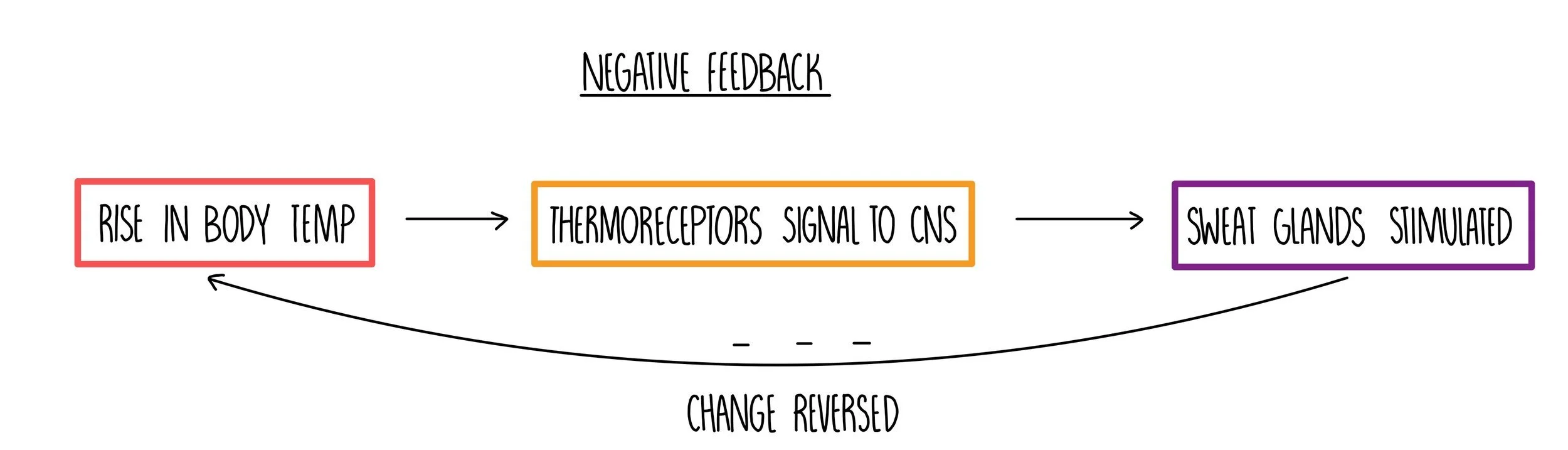
Negative and positive feedback mechanisms
Conditions within our bodies which are subject to homeostasis (such as temperature, pH and blood glucose concentration) are controlled by negative feedback mechanisms. These are mechanisms which act to reverse a change in the body - i.e. if temperature increases, a negative feedback mechanism ensures that changes to our body occurs in order to reduce our body temperature. The change in our body is detected by receptors (e.g. thermoreceptors which detect temperature or chemoreceptors which detect pH) and the reversal of the change is brought about by effectors (such as sweat glands which can modify the amount of sweat produced in order to change our body temperature). Negative feedback mechanisms therefore enable conditions within our body to remain within certain limits, fluctuating around the normal level.
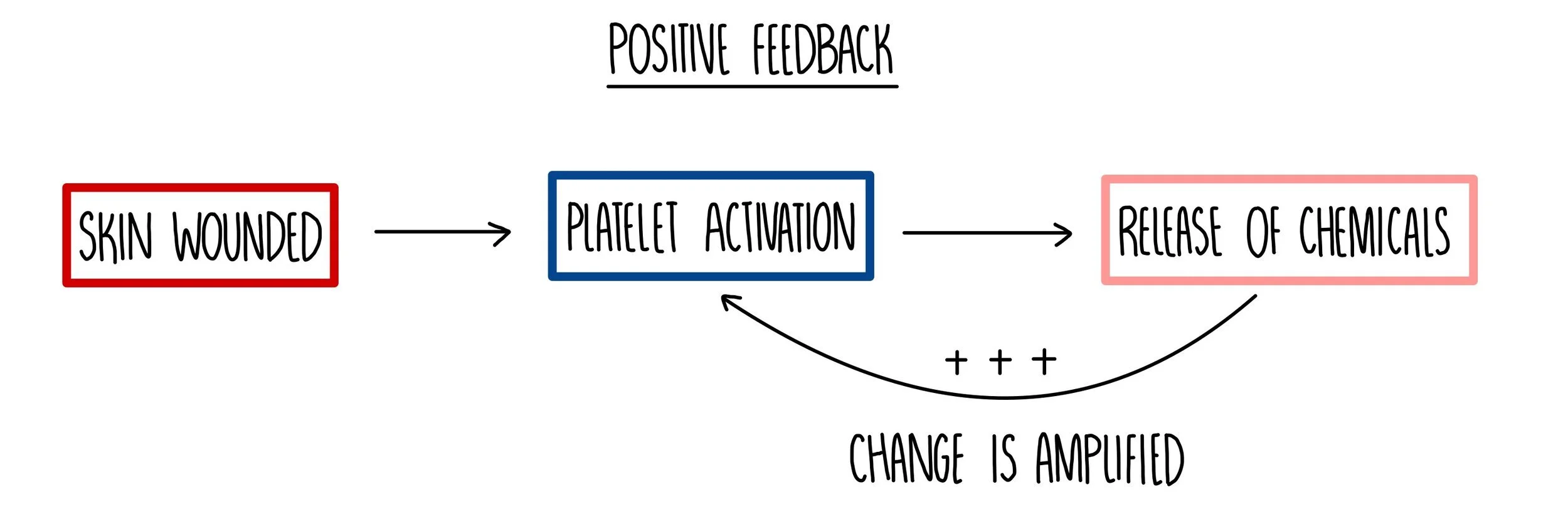
In contrast, positive feedback mechanisms will amplify a detected change, moving conditions away from the normal level. They are used to accelerate a biological pathway, for example, the formation of a blood clot after an injury. At the site of a wound, activated platelets release a chemical which results in further platelet activation. This causes platelets to rapidly accumulate at the site of the wound, forming a blood clot. Positive feedback is not involved in homeostasis, because it does not keep internal conditions within a normal range.
Control of blood glucose concentration
The concentration of glucose in the blood is one of the internal conditions that is kept constant with our bodies (homeostasis). It is monitored and controlled by the pancreas which releases a hormone called insulin if glucose levels become too high and another hormone called glucagon if levels fall too low. The action of insulin in reducing blood glucose levels and glucagon in increasing blood glucose are examples of negative feedback loops.
When blood glucose is high (i.e. after eating a meal):
Cells in the pancreas detect high blood glucose and stimulate beta cells in the islets of Langerhans to secrete insulin.
Insulin travels in the bloodstream to liver and muscle cells, where it binds to insulin receptors on their cell surface membrane.
Insulin increases the permeability of the membrane to glucose, so more glucose is moved from the bloodstream into cells. When insulin binds to its receptor, vesicles containing the GLUT4 glucose transporter move and fuse with the plasma membrane.
It also stimulates the conversion of glucose into glycogen (glycogenesis) and an increase in the rate of respiration, which helps to lower blood glucose.
When blood glucose is low (i.e. running a marathon):
Cells in the pancreas detect low blood glucose and stimulate alpha cells in the islets of Langerhans to secrete glucagon.
Glucagon travels in the bloodstream to liver cells, where it binds to glucagon receptors on their cell surface membrane.
Glucagon stimulates the breakdown of glycogen into glucose (glycogenolysis) and a decrease in the rate of respiration, which helps to increase blood glucose.
It also triggers the production of glucose from non-carbohydrates, such as lipids and amino acids, in a process called gluconeogenesis.
Adrenaline also increases blood glucose levels as part of the fight-or-flight response that prepares our body for action. It is released by the adrenal glands and binds to adrenaline receptors on the membrane of liver cells. It stimulates hydrolysis of glycogen, stimulates the secretion of glucagon and inhibits the secretion of insulin.
Second messengers
Since hormones such as adrenaline, glucagon and insulin can’t get inside target cells to exert their effects directly, they have to use second messengers to activate reactions inside cells. For example:
Adrenaline binds to its receptor on the cell surface membrane of liver cells.
This activates the enzyme adenylyl cyclase, which catalyses the production of a second messenger called cyclic AMP (cAMP).
cAMP then activates a cascade of intracellular reactions.
For example, cAMP activates an enzyme called protein kinase A, which activates a cascade which eventually leads to the breakdown of glycogen (glycogenolysis).
Diabetes
Diabetes is a condition that results from the inability to control blood glucose levels. Uncontrolled blood glucose can be dangerous, so people with diabetes have to carefully regulate their carbohydrate intake and inject themselves with precise amounts of insulin. There are two types – type 1 and type 2 diabetes.
Type 1 diabetes
Onset in childhood – some cases appear to have a genetic component, others may be triggered by viral infection.
The immune system destroys the beta cells of the islets of Langerhans so that they can no longer produce insulin.
Results in sustained hyperglycaemia (high blood glucose) after a meal. Some glucose is excreted in the urine as the kidneys cannot reabsorb all of the glucose.
Treated with insulin injections or an insulin pump. The amount of injected insulin has to be carefully controlled to prevent glucose from dropping too low.
Patients also have to follow a carefully controlled diet.
Type 2 diabetes
Onset in adulthood – linked to lifestyle factors such as poor diet, obesity and lack of exercise. Also appears to have a genetic component as it is more common in those with a family history of diabetes.
Body cells stop responding properly to insulin because their insulin receptors stop working and their cells stop absorbing glucose, leading to elevated blood glucose levels.
Treated with a managed diet and regular exercise. In more severe cases, glucose-lowering drugs or insulin injections may be used.
Type 2 diabetes is becoming more common due to increasing availability of processed foods and low levels of physical exercise.
Determining the concentration of a glucose solution
The presence of glucose in urine is an indicator of diabetes. You can measure the concentration of glucose in a urine sample by following this procedure:
Firstly, you need to make a calibration curve. Prepare serial dilutions of a concentrated glucose solution in five separate test tubes.
Add quantitative Benedict’s reagent to each solution – this is different from normal Benedict’s reagent, as it just results in the blue colour disappearing (without turning red).
Pour each solution in a cuvette and place in a colorimeter to read off the absorbance at each concentration. Plot your calibration curve with absorbance on the y-axis and glucose concentration on the x-axis.
Now take the urine sample and add quantitative Benedict’s reagent. Use the colorimeter to record the absorbance and read off the concentration of the solution using the calibration curve.
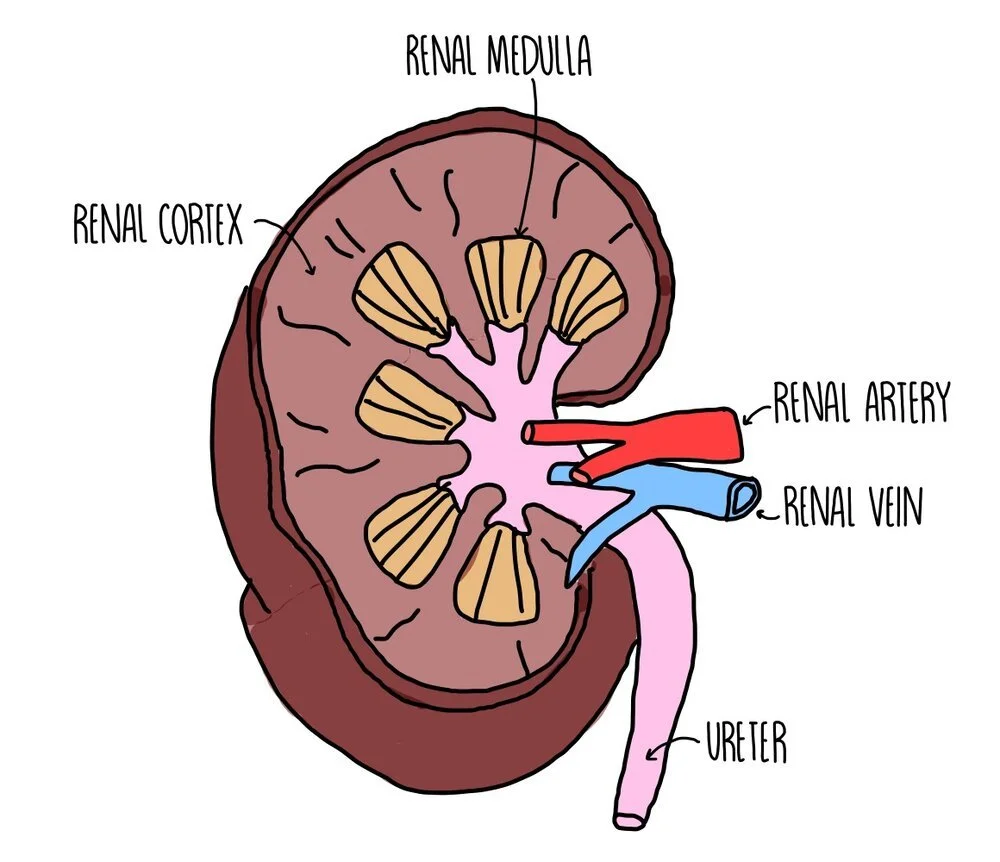
Kidneys
The inner part of the kidney is called the medulla and the outer part is the cortex. Blood is carried to the kidney via the renal artery for the kidney to filter the blood and remove waste products. The filtered blood is taken away from the kidneys by the renal vein. The individual structures which filter the blood are called nephrons.
Our kidneys remove excess water, excess ions and urea from our blood as urine. The removal of these substances from the bloodstream involves two processes: ultrafiltration and selective reabsorption.
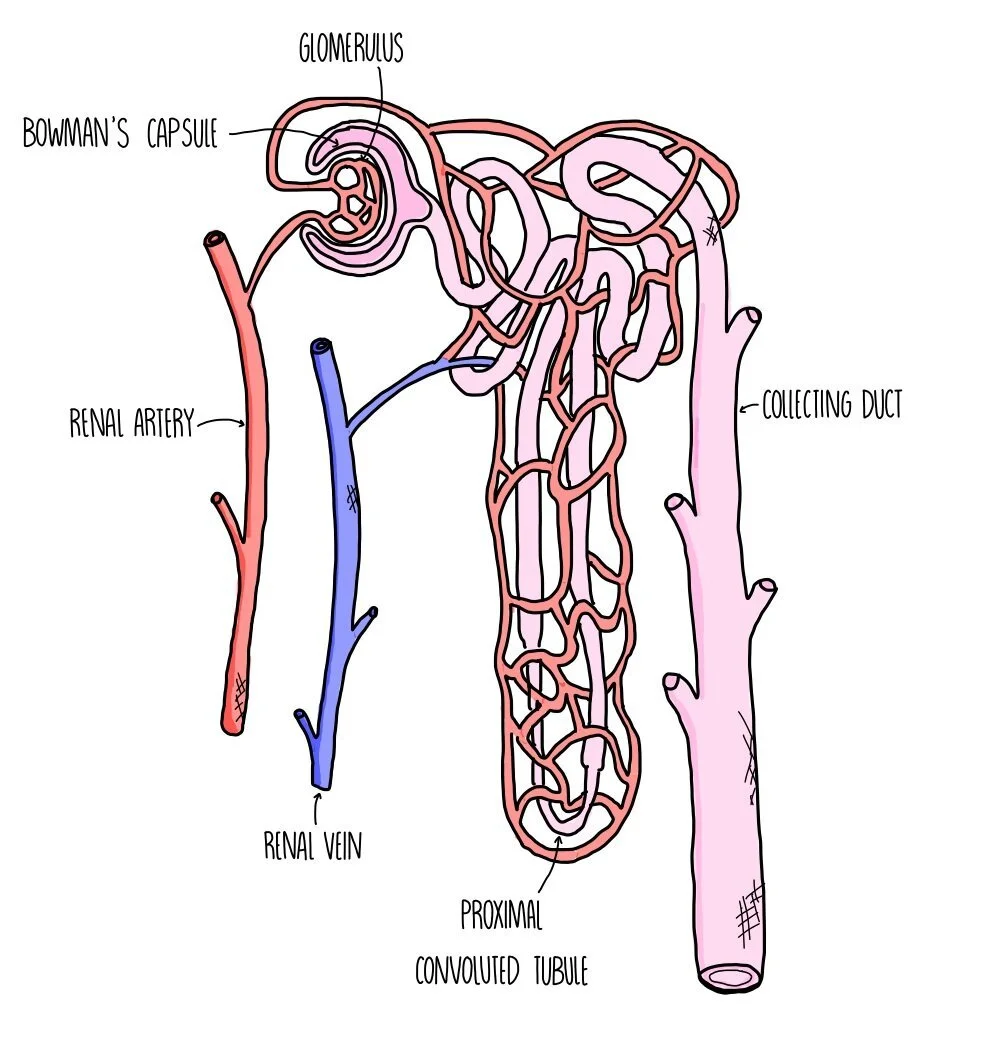
Ultrafiltration
The Bowman’s capsule surrounds a ball of capillaries called the glomerulus where blood is placed under high pressure. The efferent arteriole (leading away from the glomerulus) is smaller in diameter than the afferent arteriole (leading towards the glomerulus), so blood inside the glomerulus is under high pressure. Small molecules (glucose, urea, water and salts) are pushed out of the bloodstream and into the Bowman’s capsule, while larger molecules such as blood cells and protein stay inside the capillaries. They form a substance called glomerular filtrate, which moves through the nephron.
When small molecules pass between the capillary and the kidney, they pass through three layers: the capillary endothelium, the basement membrane and the epithelium of the Bowman’s capsule.
Selective reabsorption
In the proximal convoluted tubule (PCT), loop of Henle and the distal convoluted tubule (DCT), useful substances are reabsorbed, passing out of the nephron and back into the capillaries. Glucose is reabsorbed in the PCT by active transport and facilitated diffusion. The PCT epithelium has microvilli to provide a large surface area for reabsorption. Water is reabsorbed in the loop of Henle, DCT and collecting duct by osmosis. The remaining filtrate is urine, containing excess water, excess salts and urea. This passes from the collecting duct to the bladder via the ureter. Urine may contain additional substances like hormones, excess vitamins, the breakdown products of medications and recreational drugs.
Water reabsorption
Water is reabsorbed along almost the entirety of the nephron, but regulation of water potential mostly takes place in the DCT, loop of Henle and collecting duct with the amounts of water reabsorbed controlled by hormones such as ADH.
The nephron spans two parts of the kidney – the Bowman’s capsule, PCT and DCT are in the cortex of the kidney while the loop of Henle and lower half of the collecting duct are located in the medulla. The loop of Henle is made up of two limbs called the ascending and descending limb, which control the movement of ions and allow water to be reabsorbed:
The ascending limb is permeable to ions but impermeable to water. At the top of the ascending limb, sodium ions are actively pumped into the medulla.
This lowers the water potential of the medulla, causing water to move out of the nephron by osmosis from the descending limb (which is permeable to water but not ions).
As water moves out of the nephron, the filtrate becomes more concentrated. This causes sodium ions to move out of the nephron at the start of the ascending limb, down their concentration gradient by facilitated diffusion.
This lowers the water potential of the medulla even further, causing water to move out of the DCT and collecting duct by osmosis.
Water that has moved into the medulla eventually moves into the capillary.
Organisms that live in dry conditions (e.g. camels) are adapted by having an extra-long loop of Henle. This means that more ions can be pumped into the medulla, encouraging more water to move out of the nephron by osmosis.
Antidiuretic hormone (ADH)
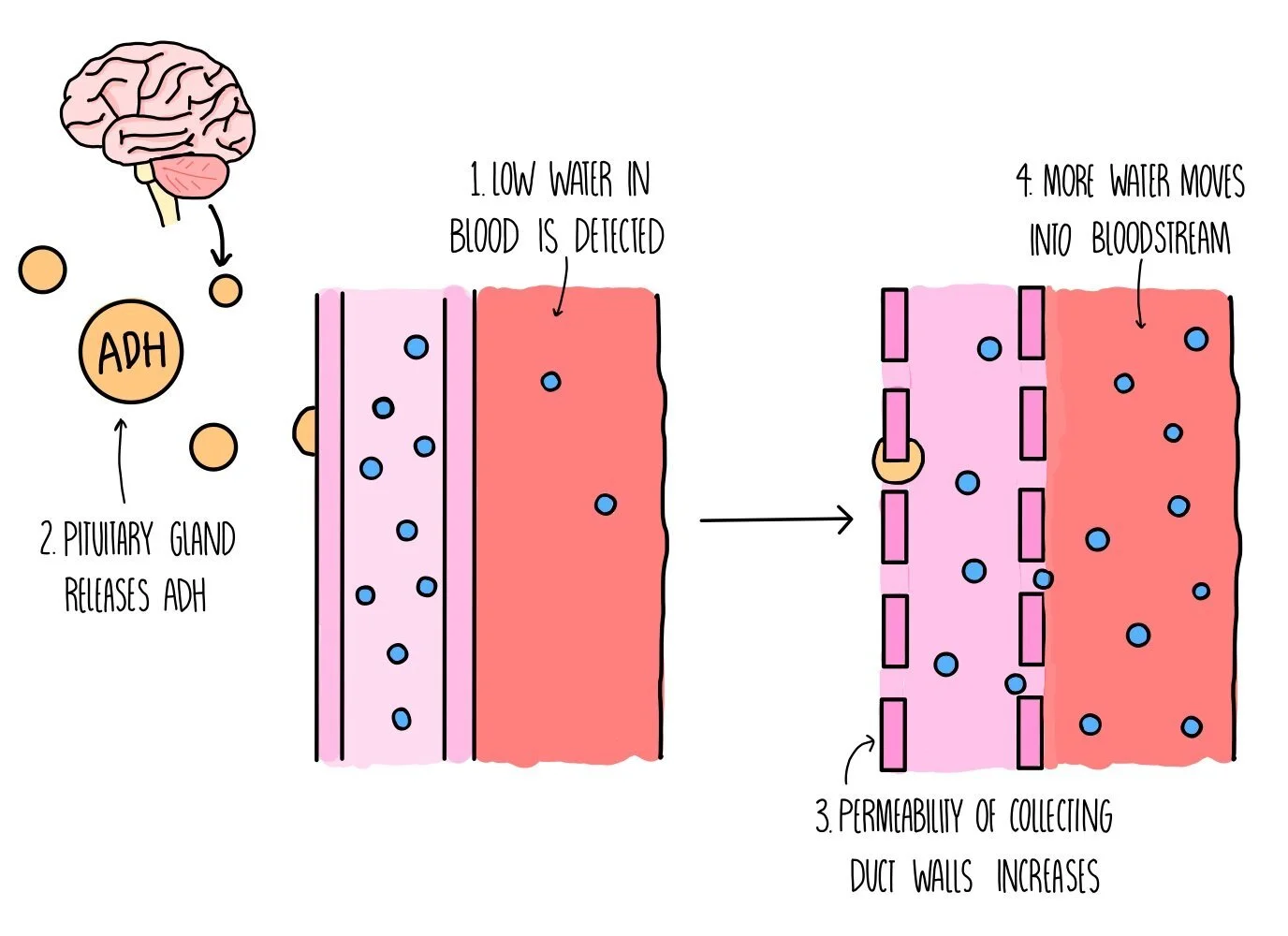
ADH controls the water content of our urine by increasing the reabsorption of water from the collecting duct. It works by increasing the permeability of the collecting duct wall, making it more porous and allowing more water to pass from the kidney into the bloodstream. It is released by the pituitary gland in the brain when water levels in our blood plasma are becoming low. This type of control is an example of a negative feedback mechanism:
Osmoreceptors in the hypothalamus detect a drop in blood water potential.
The hypothalamus signals to the posterior pituitary gland to secrete ADH.
ADH causes the walls of the DCT and collecting duct to become more permeable to water (by the incorporation of more aquaporins into the membranes of the cells that line these parts of the nephron).
More water moves by osmosis out of the DCT/collecting duct and reabsorbed into the bloodstream, increasing its water potential.
A smaller volume of concentrated urine is produced.