Immune Response
Pathogens
A pathogen is any organism which causes disease. Infectious diseases are always caused by pathogens, which can spread from person to person to infect others. Non-infectious diseases, such as lung cancer or diabetes, are not caused by pathogens and tend to be more influenced by genetics or lifestyle factors.
Pathogens include bacteria, viruses, protoctists and fungi. Here are some examples of pathogenic organisms from each of these kingdoms:
Bacteria - Mycobacterium tuberculosis causes TB
Virus - HIV causes AIDS, COVID-19 causes coronavirus, the influenza virus causes seasonal flu
Protoctist - Plasmodium causes malaria
Fungi - Trichophyton causes Athlete’s foot
Bacterial cell structure
Bacteria are single-celled prokaryotic organisms which contain the following structures:
Circular chromosomal DNA – floats free in the cytoplasm.
Ribosomes – these are smaller than those found in eukaryotic cells (70S)
Cell wall - made of murein (a glycoprotein)
Pili - pili are hair-like structures which stick out from the plasma membrane. They are used to communicate with other cells (including the transfer of plasmids between bacteria).
Mesosomes - the mesosome is a folded portion of the inner membrane. While some scientists believe that it plays a role in chemical reactions, such as respiration, other scientists doubt whether it even exists and think that it may just be an artefact produced during the preparation of bacterial samples for microscopy.
Plasmids - plasmids are small, circular rings of DNA which are separate from the main chromosome. They house genes which are not crucial for survival but might prove useful - such as antibiotic-resistance genes, for example. Plasmids can replicate independently from the main chromosomal DNA.
Slime capsule - in addition to a cell wall, some bacteria also have a capsule which is made of slime. The main function of the capsule is to protect the bacterium against an immune system attack.
Flagellum – rotates to move the bacterium
HIV and AIDS
Human immunodeficiency virus (HIV) is a deadly virus which can weaken a person’s immune system by destroying a type of immune cell called T helper cells. It is spread through the transmission of infected bodily fluids (e.g. during sexual intercourse, sharing of needles or blood transfusion). HIV doesn’t kill the patient directly, but weakens the immune system to an extent that the patient is unable to fight off other infections which normally would not pose a threat - these are known as opportunistic infections.
When the patient’s immune system has weakened to a particularly low level (this is seen by a low T helper cell count in hospital blood tests), the patient has developed a disease called acquired immunodeficiency syndrome (AIDS). The time between the initial infection and the onset of AIDS symptoms (the latency period) varies greatly between individuals but is usually around 10 years. The length of the latency period depends on the individual’s age, strength of their immune system and access to healthcare.
The symptoms of AIDS follow a series of stages:
The person will first develop less serious, minor infections which will gradually become more and more severe.
As the patient’s body tries to fight off more infections, the lower their T cell levels drop.
Eventually their immune system will be so weak that they will die of an opportunistic infection because they do not have enough immune cells to defend themselves.
HIV replication
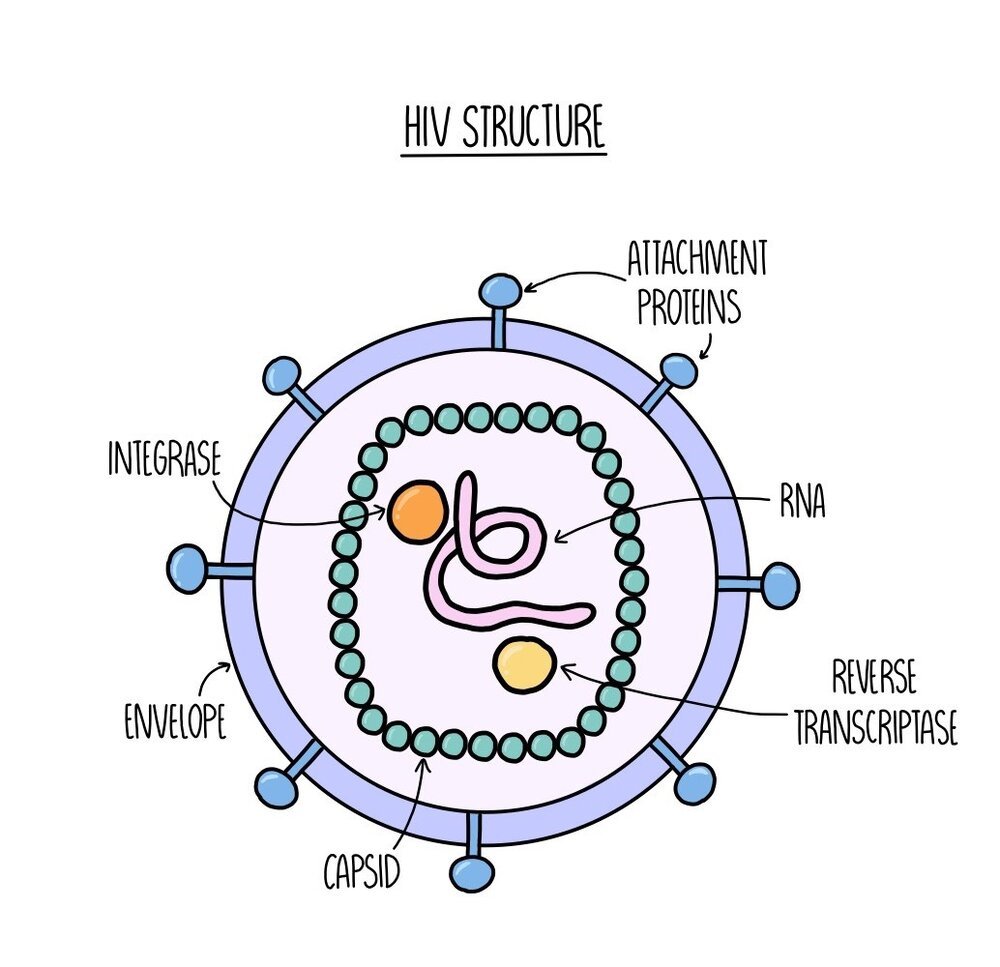
The HIV virus consists of a core of RNA and enzymes (reverse transcriptase and integrase) which is enclosed in a protein coat called a capsid. Surrounding the capsid is an outer layer called the envelope which contains attachment proteins - these proteins are crucial for the virus to enter host cells (they act like little keys to access our cells).
If a person with HIV exchanges bodily fluid with another person, HIV can infect the second individual and will be present in their bloodstream. The HIV virus uses its attachment proteins to enter human immune cells (specifically the T helper cell) by binding to receptors on the T cell. The capsid is released into the cell, where it breaks apart to release the RNA and enzymes. The enzyme reverse transcriptase converts the RNA into DNA. The single-stranded DNA is converted into double-stranded DNA which the enzyme integrase can insert into the DNA of the T cell. The T cell now has the ‘instructions’ (genes) to produce viral proteins. The viral DNA is transcribed and translated and the viral proteins are used to build new virus particles, which move out of the T cell and infect other cells.
Tuberculosis (TB)
TB is caused by a bacterium called Mycobacterium tuberculosis. It is spread through lipid droplets i.e. when an infected person sneezes or coughs. The lipid droplets are inhaled by another person, causing the bacteria to move into the lungs. Once they are in the lungs, the bacteria are engulfed by a type of white blood cell called a phagocyte. Phagocytes usually work by digesting and killing the pathogen, but Mycobacterium tuberculosis is able to disrupt this process. The bacteria are able to survive and replicate from inside the phagocytes.
The time between infection with M. tuberculosis and the onset symptoms can vary between individuals - there is a latency period between a few weeks to many years. Initial symptoms include a cough and fever which is caused by inflammation of the lungs. The lungs become progressively more damaged, leading to respiratory failure and sometimes death. It can also spread to other parts of the body, such as the kidneys and the brain.
Often the symptoms of TB do not appear immediately. Our body is able to seal off infected phagocytes inside structures within our lungs called tubercles. The bacteria within the tubercles lie dormant for a period lasting up to a few years. The bacteria then become reactivated - reactivation can be stimulated by a weakened immune system (e.g. due to AIDS).
Barriers to prevent entry of pathogens
Our bodies have several defensive barriers to prevent us becoming infected by pathogens. For example:
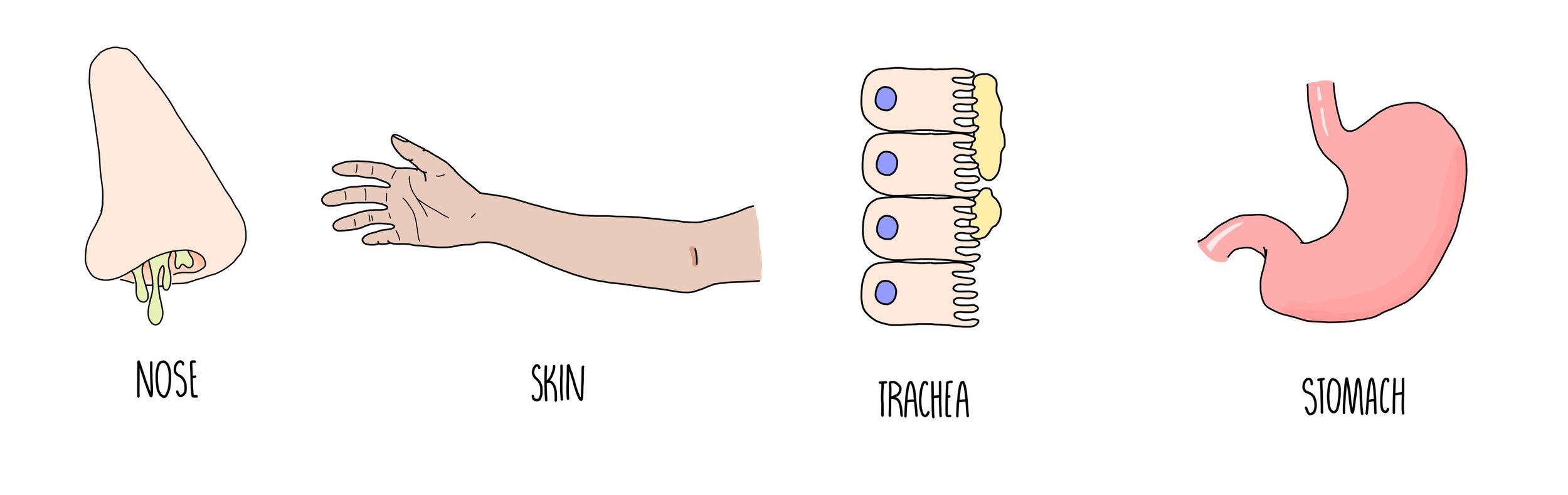
Our body cavities (e.g. eyes, nose, mouth, genitals) are lined with a mucus membrane which contains an enzyme called lysozyme. Lysozyme kills bacteria by damaging their cell walls, causing them to burst open.
Our skin acts as a physical barrier to stop pathogens from getting inside of us. If our skin is cut or wounded, our blood quickly clots to minimise the entry of pathogens.
The trachea (windpipe) contains goblet cells which secrete mucus. Pathogens that we inhale become trapped in the mucus, which is swept towards the stomach by the action of ciliated epithelial cells.
Our stomach contains gastric juices which are highly acidic - these will denature proteins and kill any pathogens that have been ingested in our food and drinks.
The insides of our intestines and the surface of our skin are covered in harmless bacteria which will compete with any pathogenic organisms and reduce their ability to grow.
Non-specific immune response
The non-specific immune response is our immediate response to infection and is carried out in exactly the same way regardless of the pathogen (i.e. it is not specific to a particular pathogen). The non-specific immune response involves inflammation, the production of interferons and phagocytosis.
Inflammation - the proteins which are found on the surface of a pathogen (antigens) are detected by our immune system. Immune cells release molecules to stimulate vasodilation (the widening of blood vessels) and to make the blood vessels more permeable. This means that more immune cells can arrive at the site of infection by moving out of the bloodstream and into the infected tissue. The increased blood flow is why an inflamed part of your body looks red and swollen.
Production of interferons - if the pathogen which has infected you is a virus, your body cells that have been invaded by the virus will start to manufacture anti-viral proteins called interferons. They slow down viral replication in three different ways:
Stimulate inflammation to bring more immune cells to the site of infection
Inhibit the translation of viral proteins to reduce viral replication
Activate T killer cells to destroy infected cells
Phagocytosis
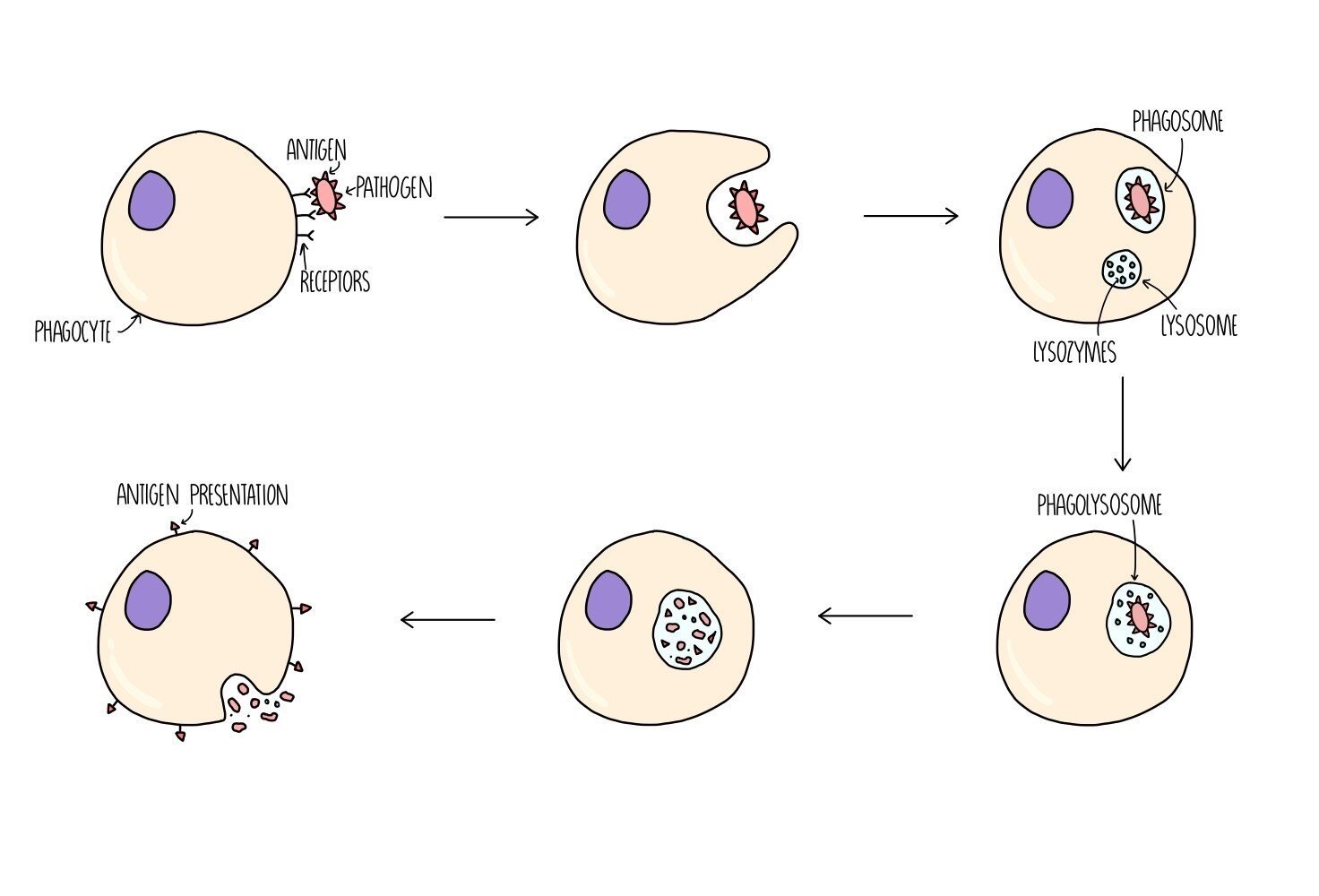
Phagocytes are a type of white blood cell which can destroy pathogens - types of phagocyte include macrophages, monocytes and neutrophils. They first detect the presence of the pathogen when receptors on its cell surface bind to antigens on the pathogen. The phagocyte then wraps its cytoplasm around the pathogen and engulfs it. The pathogen is contained within a type of vesicle called a phagosome. Another type of vesicle, called a lysosome, which contains digestive enzymes (lysozymes) will fuse with the phagosome to form a phagolysosome. Lysozymes digest the pathogen and destroy it. The digested pathogen will be removed from the phagocyte by exocytosis but they will keep some antigen molecules to present on the surface of their cells - this serves to alert other cells of the immune system to the presence of a foreign antigen. The phagocyte is now referred to as an antigen-presenting cell (APC).
Specific immune response
The specific immune response happens after the non-specific response and is an attack aimed at a particular antigen. It involves the activation of two types of immune cells: T lymphocytes and B lymphocytes.
T lymphocyte response
T lymphocytes are white blood cells which contain receptors on their cell surface. Different T cells have different shaped receptors on their surface (so they will each bind to a different-shaped antigen). When a particular T cell binds to a complementary antigen (e.g. on a antigen-presenting cell or on a pathogen), the T cell will become activated - this is called clonal selection. Once it is activated, the T cell divides by mitosis to produce clones of itself - this is called clonal expansion. There are different types of T cell which play different roles in the immune response:
T helper cells release chemicals (they release a type of cytokine called interleukins) to activate B lymphocytes.
T killer cells destroy any cells which have been infected with the pathogen.
T regulatory cells suppress other immune cells and prevent them from attacking our own (host) cells.
T memory cells remain in the bloodstream in low levels in case reinfection occurs. If the antigen is detected again at a later date, they will divide into T helper, T killer and T regulatory cells.
B lymphocyte response
B cells are activated when chemicals are released from T helper cells. They are also activated when the antibody molecules on their cell surface bind to a complementary antigen. Different B cells have different shaped antibodies on their surface, so only the B cells with the correct-shaped antibodies will be activated. Once they are activated, the B cells divide by mitosis and differentiate into two kinds of cell - plasma cells and memory cells.
Plasma cells produce antibodies with a complementary shape to the antigen.
Memory cells remain in the bloodstream in low levels in case reinfection occurs. If the antigen is detected again at a later date, they will quickly divide into plasma cells.
Antibody structure
Antibodies have a quaternary structure made up of four polypeptide chains (two heavy chains and two light chains) held together by disulfide bridges. They are composed of a variable region (which is different in different antibodies) where the antigen-binding site is located. The antigen-binding site has a complementary shape to the antigen which makes it specific to that particular antigen. There is also the constant region which is the same for all antibodies. The constant region contains another binding site which allows the antibody to bind to immune system cells, such as B cells or phagocytes. In between the variable region and the constant region is the hinge region which provides the antibody with flexibility.
How antibodies work
Antibodies work to destroy pathogens in three different ways.
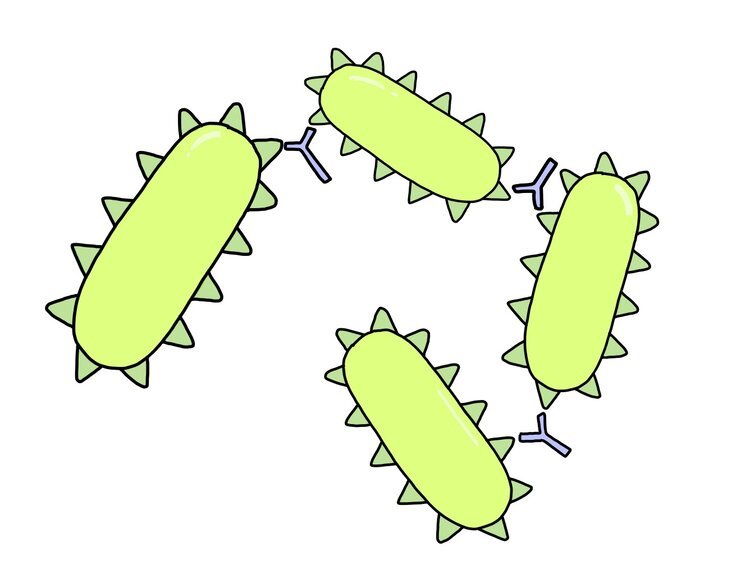
Agglutination - antibodies each contain two antigen-binding sites which means they can bind to two pathogens at the same time. This causes pathogens to become clumped together. Phagocytes can then engulf and digest lots of pathogens at the same time, which makes phagocytosis more efficient.
Neutralising toxins - certain pathogens, such as bacteria, make us feel ill by releasing toxins. Antibodies can bind to toxins which renders them harmless (it neutralises them). The antibody-toxin complex can then be destroyed by phagocytes.
Blocking access to human cells - pathogens enter host cells when their antigens bind to receptor molecules on host cells (like a key opening a lock). When antibodies bind to antigens, it prevents the antigen from fitting in the receptor which means it can’t get inside the cell.
Membrane-bound and secreted antibodies
Antibodies can either be membrane-bound (e.g. found on the surface of B cells) or secreted by plasma cells and float freely in the bloodstream. The heavy chains of these two types of antibody differ slightly - the heavy chains of membrane-bound antibodies contain an extra region which enables attachment to the cell membrane.
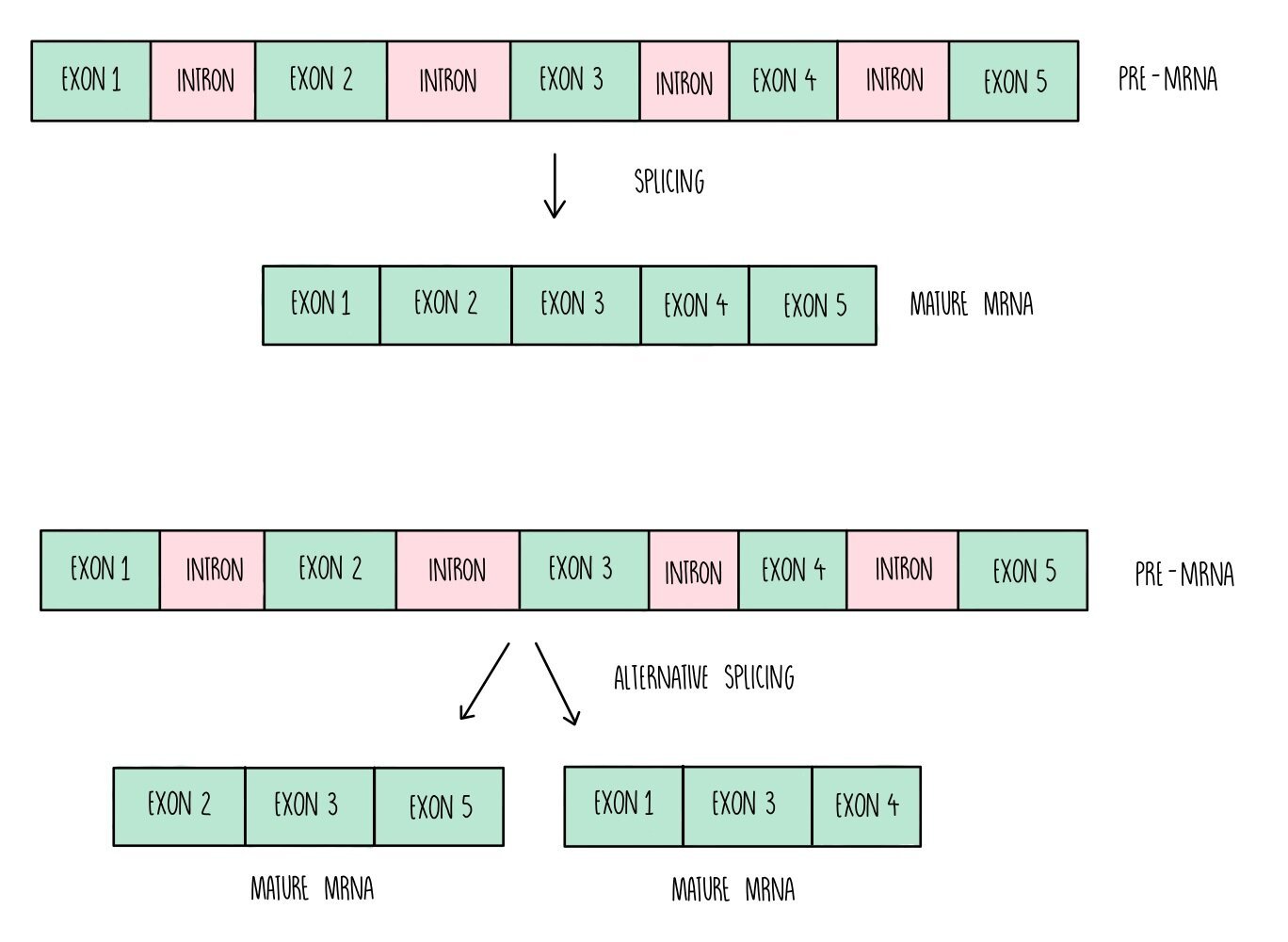
The heavy chains for both antibodies are produced from the same gene. A gene can produce two (or more) different proteins through a process called alternative splicing. Splicing is a process where the non-protein coding parts of a gene (the introns) are snipped out and the protein-coding regions (the exons) are stuck together to form a mature mRNA molecule. Certain genes will splice their exons in different combinations, so that different proteins are produced. Alternative splicing means that multiple proteins can be produced from the same gene and explains why organisms display a huge number of proteins from a relatively small number of genes.
Primary and secondary immune response
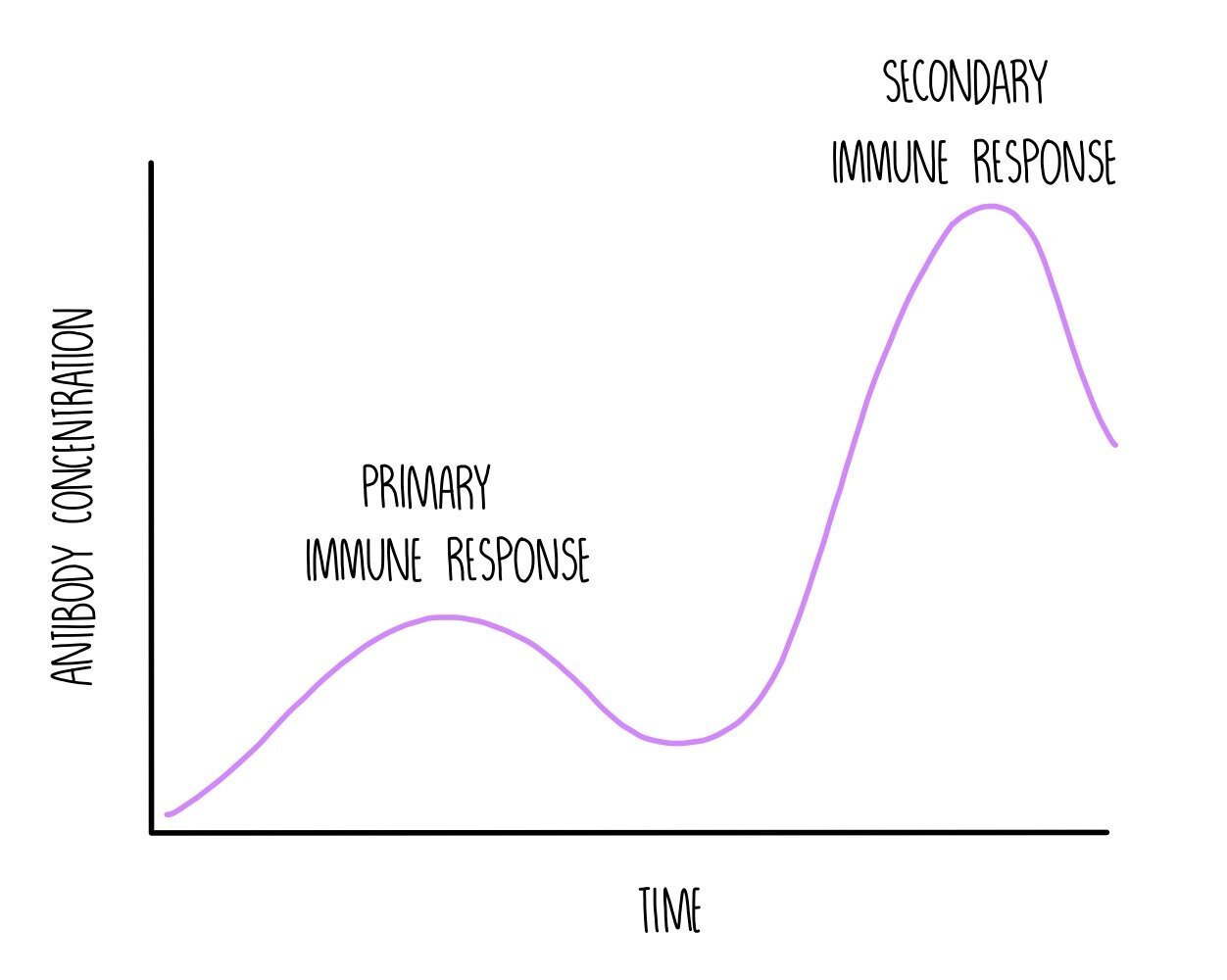
The primary immune response occurs when you are infected with a pathogen for the first time. It is composed of the non-specific and the specific immune response. This process is slow because it takes time for the correct B cell to be activated (clonal selection) and divide into lots of plasma cells (clonal expansion) in order to produce antibodies with a complementary shape to the antigen. The infected person will experience symptoms while the T and B cells mount an immune response. As part of the primary response, both T and B cells produce memory cells.
If you are re-infected with the same pathogen in the future, the T and B memory cells will recognise the antigen and start dividing. T memory cells will divide into the correct type of T killer cell to kill any cells that are infected with the pathogen. B memory cells will divide into plasma cells to produce a large number of antibodies which is complementary to the antigen molecules on the pathogen. This is the secondary immune response and is much quicker than the primary response. It happens so quickly that the pathogen is suppressed before you are able to experience symptoms - you are immune to the pathogen.
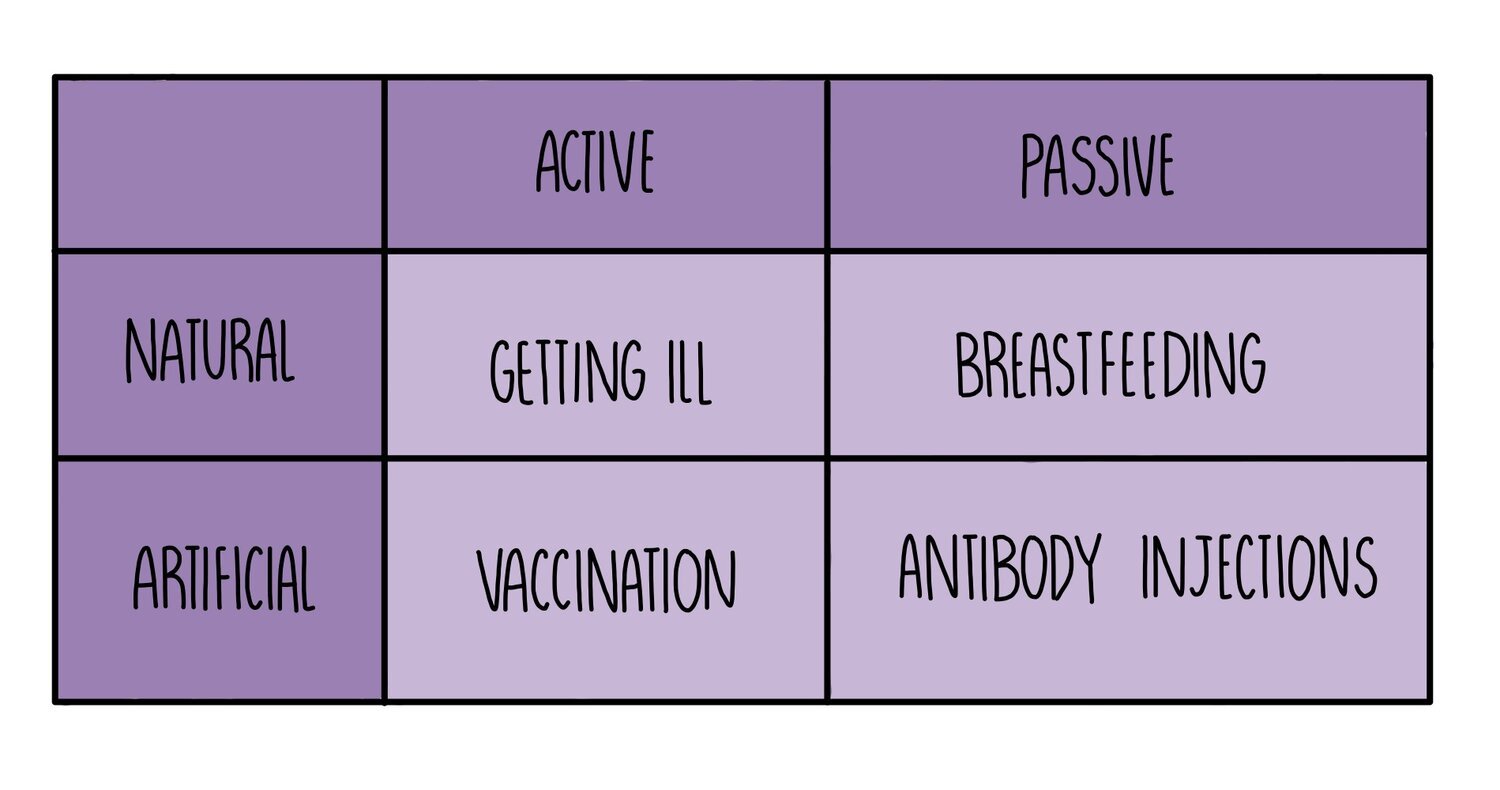
Active vs passive immunity
Active immunity occurs when your body makes its own antibodies after being stimulated by an antigen. This process can be natural (e.g. if you catch a cold, your body will make its own antibodies against the common cold virus) or it can be artificial (e.g. if you are vaccinated with a harmless form of an antigen).
Passive immunity occurs when you are given ready-made antibodies that have been produced by another organism. This process can be natural (e.g. babies receive antibodies from their mother when they breastfeed) or artificial (e.g. antibody injections can be given for some diseases - e.g. this is being tested as a treatment for Ebola).
Active immunity lasts longer since memory cells will remain in the body for years but it takes time to develop. Passive immunity provides immediate protection against pathogens but is short-lived (antibodies that are transferred from mother to child during breastfeeding only remain in the body for about 18 months).
Vaccines
Vaccines contain a dead or weakened form of a pathogen which is injected into the bloodstream. Sometimes vaccines contain just the antigen proteins without the rest of the pathogen. Other vaccines might contain a variety of different antigens to protect against different strains of pathogens which vary in the shape of the proteins on their cell surface membranes (antigenic variation). The injection of weakened antigens stimulates a primary immune response and the production of memory T cells and memory B cells, resulting in immunity without becoming ill from the disease.
Evasion mechanisms
Our immune systems have evolved to increase our defence against pathogens. As this has happened, pathogens have also evolved to become better at infecting us. This is known as an evolutionary race. For example, the HIV virus has evolved certain evasion mechanisms to escape detection by our immune system:
HIV has a high rate of mutation in the genes which code for its antigens. This means that different strains of HIV will show slight differences in the shape of their antigens (antigenic variation). Memory cells that have formed from one HIV strain therefore may not detect the presence of antigens from other HIV strains.
HIV replicates inside T lymphocytes and destroy the cells when they burst out of them. This disrupts the person’s immune response because their T cell levels will be too low to produce an effective immune response against the virus.
HIV disrupts antigen presentation in host cells which prevents the activation of T helper cells.
The bacterium responsible for TB, Mycobacterium tuberculosis also has ways in which it evades our immune system:
When M. tuberculosis gets inside the lungs, it is engulfed by phagocytes as part of the non-specific immune response. Phagocytes usually kill pathogens by digesting them but the M. tuberculosis bacterium is able to stop this by preventing the phagosome from fusing with the lysosome. The bacteria are able to survive and replicate inside the phagocyte.
M. tuberculosis disrupts antigen presentation in host cells which prevents the activation of T helper cells.
Antibiotics
Antibiotics are substances which prevent the growth of bacteria. There are two types of antibiotics - bactericidal antibiotics which kill bacterial cells and bacteriostatic antibiotics which inhibit the growth of bacteria. They work by either damaging the cell wall or preventing protein synthesis:
Antibiotics can prevent bonds forming between the murein (peptidoglycan) molecules which make up the cell wall. This weakens the cell wall and prevents bacterial cells from growing properly. If water enters the bacterial cell by osmosis, the weakened cell wall cannot withstand the increased hydrostatic pressure and can burst (lysis), killing the bacteria.
Antibiotic molecules bind to bacterial ribosomes and prevent them from carrying out translation. This prevents the synthesis of enzymes (which are proteins), which catalyse important metabolic reactions. If these metabolic reactions do not take place, the bacterial cell cannot grow and reproduce properly.
This explains why antibiotics have no effect on eukaryotic cells (such as human cells) since eukaryotic cells do not have a cell wall and their ribosomes are a different size (which means that antibiotics cannot bind to them). Similarly, antibiotics have no effect on viruses because they do not possess either a cell wall or ribosomes. This is why it would be pointless prescribing antibiotics for a viral infection, such as measles or the flu.
Preparing plant extracts for antimicrobial testing
Some plants, including garlic, mint and turmeric, contain natural antibiotic molecules and can inhibit the growth of microorganisms. There are loads of other plants in the world which haven’t been tested and may also have antimicrobial properties - this is one of the reasons why maintaining plant biodiversity is so important. These compounds can be extracted and used to manufacture antibiotic drugs.
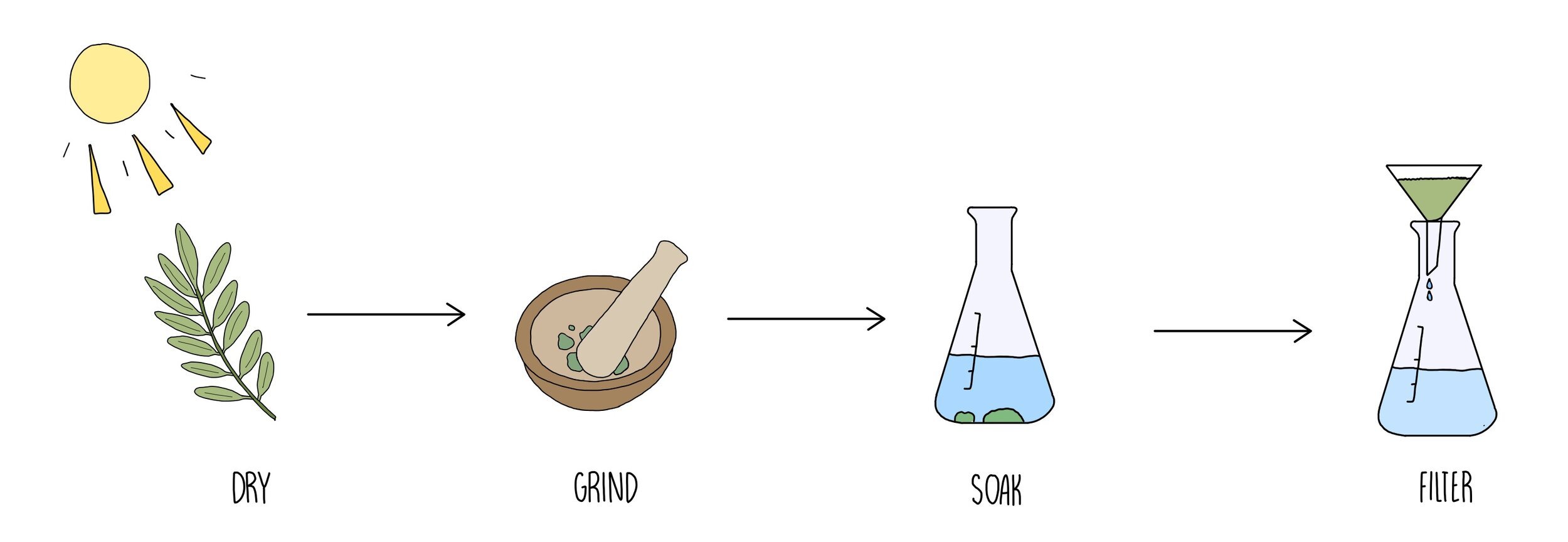
In order to test a plant for antimicrobial properties, you will first have to prepare a plant extract using the following method:
Dry out the plant by leaving in the sun until the water has evaporated out then grind using a pestle and mortar.
Soak the ground plant tissue in ethanol - this will extract the antimicrobial substances which are soluble in ethanol.
Filter the solution to remove the pieces of plant tissue. Keep the solution containing the dissolved plant extract.
Testing antibiotics
The efficiency of different antibiotics (or plant extracts containing antimicrobial substances) can be tested by soaking pieces of filter paper in the antibiotic solutions and placing on a Petri dish containing bacteria. The stronger the antibiotic, the more bacteria are killed. Regions of the Petri dish where bacteria have been killed will appear as a clear zone - the size of the clear zone is proportional to the strength of the antibiotic. The experiment is carried out by carrying out the steps below:
Prepare a nutrient broth containing bacteria and add the same volume of the broth to a series of Petri dishes.
Using a sterile plastic spreader, spread the bacterial broth evenly across the Petri dish. Remember to keep the lid on the Petri dish wherever possible.
Using sterile forceps, place a disc of filter paper into each antibiotic solution then place far apart on the Petri dish. It is important to keep all control variables (soaking time and size of the disc) the same for each antibiotic.
Incubate the Petri dishes at 25oC for 24 - 48 hours. It is important that the temperature is not higher (anywhere around 37oC) since this would pose the risk of growing human pathogens.
Measure the area or the diameter of each clear zone.
Repeat the experiment at least three times and calculate the mean area of the clear zone for each antibiotic.
Aseptic Techniques
When carrying out experiments involving bacteria, it is important to carry out aseptic (sterile) techniques. This is because bacteria are everywhere and you don’t want cross-contamination to interfere with your results. Aseptic techniques include the following:
Use of sterile equipment - this can be done using a machine called an autoclave which looks like a dishwasher but uses steam and high pressure to sterilise the equipment.
Disinfect the lab bench and work surfaces.
Wear gloves.
Place a Bunsen burner near to your work space when transferring bacteria from one container to another. The heat from the flame draws any microorganisms in the air away from the work space because hot air rises.
Close windows and doors to prevent draughts blowing microbes towards you.
Hospital acquired infections (HAIs)
HAIs are infections which are transmitted in hospital. They spread as a result of poor hygiene practices and can spread easily in hospitals because patients have weakened immune systems. The spread of HAIs can be prevented by good hygiene practices, such as hand washing and sterilising surgical equipment. Infections caused by antibiotic-resistant bacteria such as MRSA are particularly dangerous forms of HAIs because they cannot be treated by antibiotics. Hospitals put measures in place to prevent the development of antibiotic resistance, including:
The rotated use of different antibiotics
Taking the full course of antibiotics
Avoiding overuse of antibiotics (e.g. for minor infections or for viral diseases).