The Immune System
Pathogens and antigens
Pathogens are organisms which cause disease. They possess molecules (usually proteins) on their cell surface called antigens which trigger an immune response when detected by our immune system. When an antigen is detected, the immune response undergoes four main stages: phagocytosis of pathogen, activation of T lymphocytes, activation of B lymphocytes and production of antibodies by plasma cells.
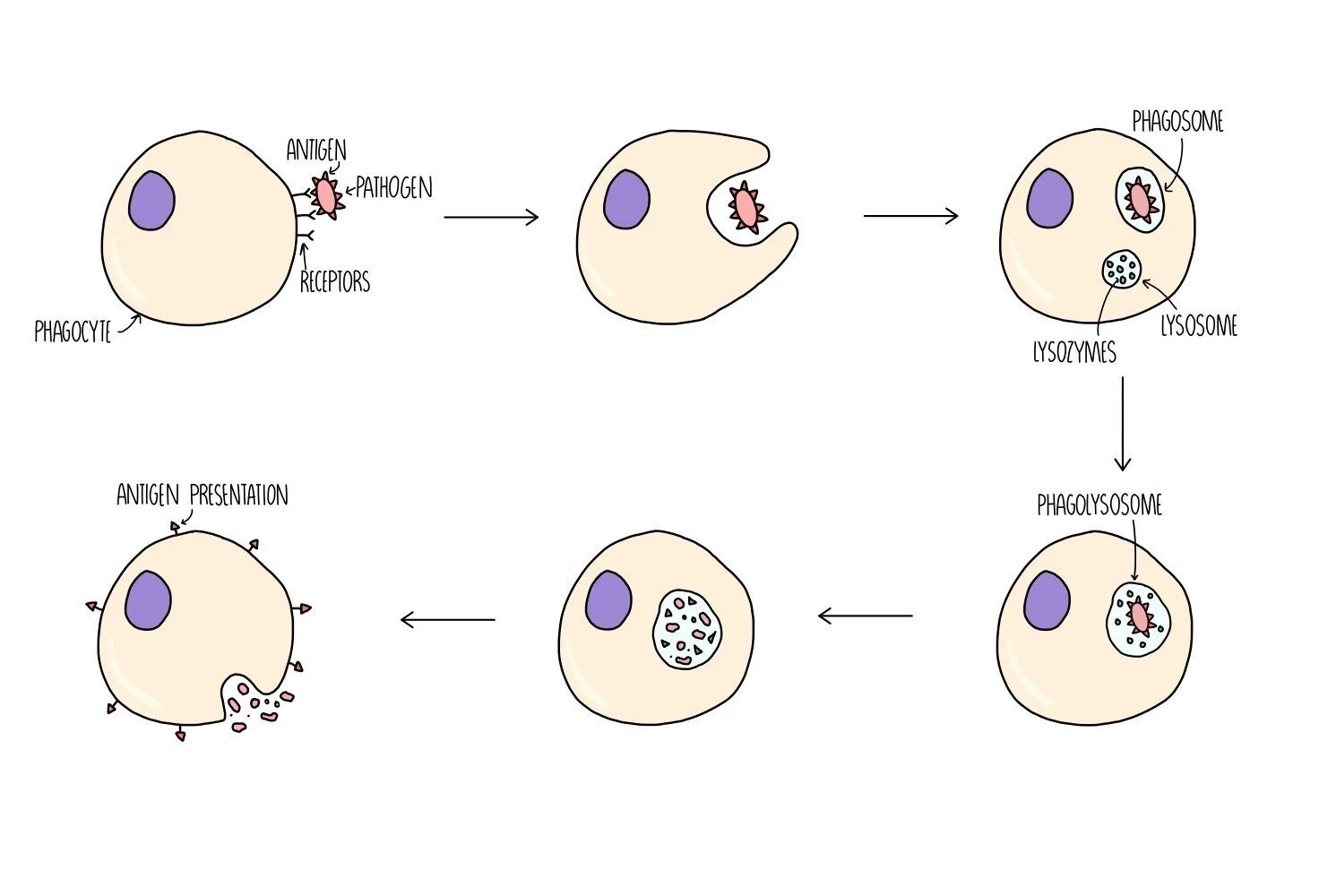
Phagocytosis
Phagocytes are a type of white blood cell which can destroy pathogens - types of phagocyte include macrophages, monocytes and neutrophils. They first detect the presence of the pathogen when receptors on its cell surface bind to antigens on the pathogen. The phagocyte then wraps its cytoplasm around the pathogen and engulfs it. The pathogen is contained within a type of vesicle called a phagosome. Another type of vesicle, called a lysosome, which contains digestive enzymes (lysozymes) will fuse with the phagosome to form a phagolysosome. Lysozymes digest the pathogen and destroy it. The digested pathogen will be removed from the phagocyte by exocytosis but they will keep some antigen molecules to present on the surface of their cells - this serves to alert other cells of the immune system to the presence of a foreign antigen. The phagocyte is now referred to as an antigen-presenting cell (APC).
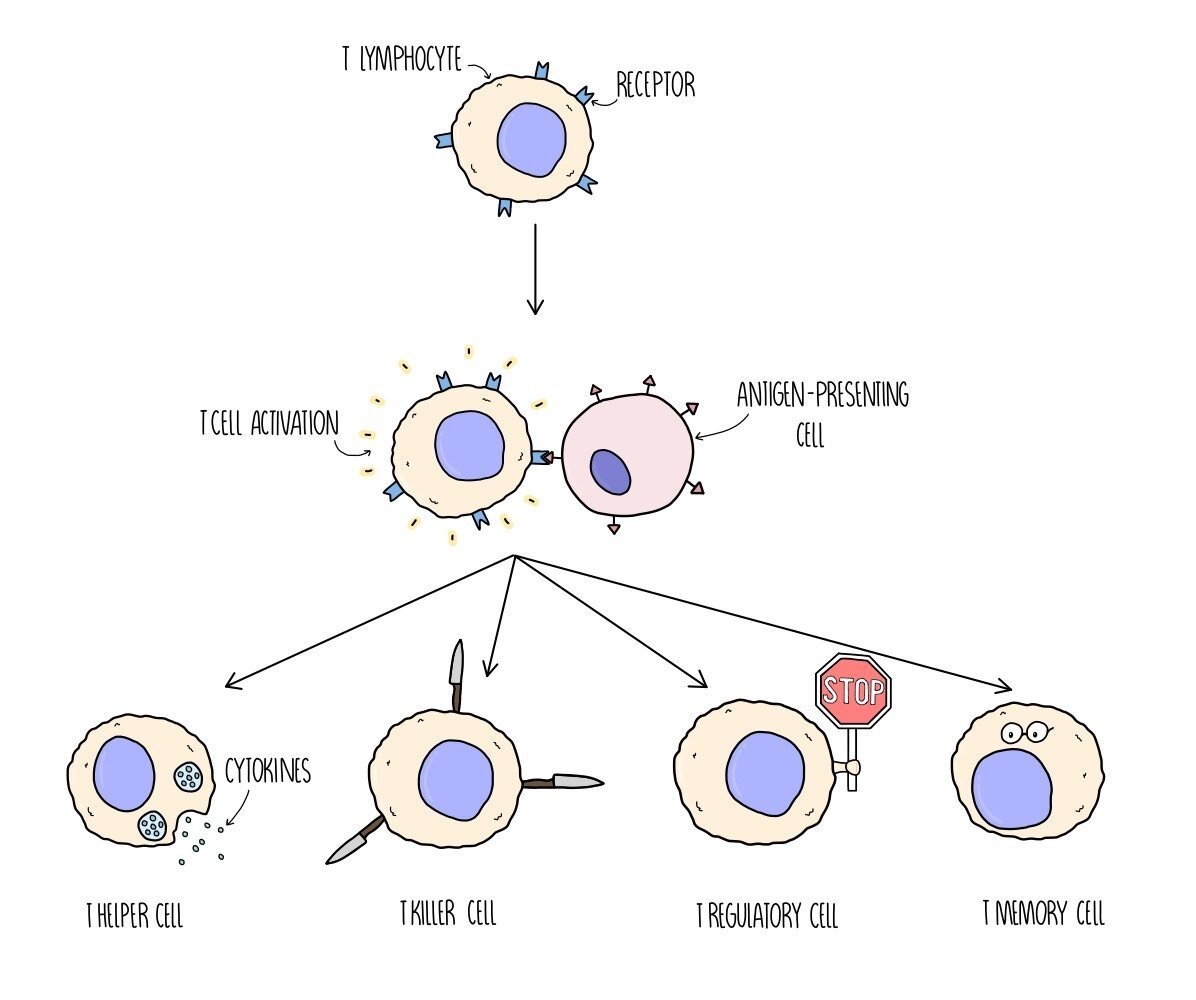
T lymphocyte response
T lymphocytes are white blood cells which contain receptors on their cell surface. Different T cells have different shaped receptors on their surface (so they will each bind to a different-shaped antigen). When a particular T cell binds to a complementary antigen (e.g. on a antigen-presenting cell or on a pathogen), the T cell will become activated - this is called clonal selection. Once it is activated, the T cell divides by mitosis to produce clones - this is called clonal expansion. There are different types of T cell which play different roles in the immune response:
T helper cells release chemicals (they release a type of cytokine called interleukins) to activate B lymphocytes.
T killer cells (aka cytotoxic T cells) destroy any cells which have been infected with the pathogen.
T regulatory cells suppress other immune cells and prevent them from attacking our own (host) cells.
T memory cells remain in the bloodstream in low levels in case reinfection occurs. If the antigen is detected again at a later date, they will divide into T helper, T killer and T regulatory cells.
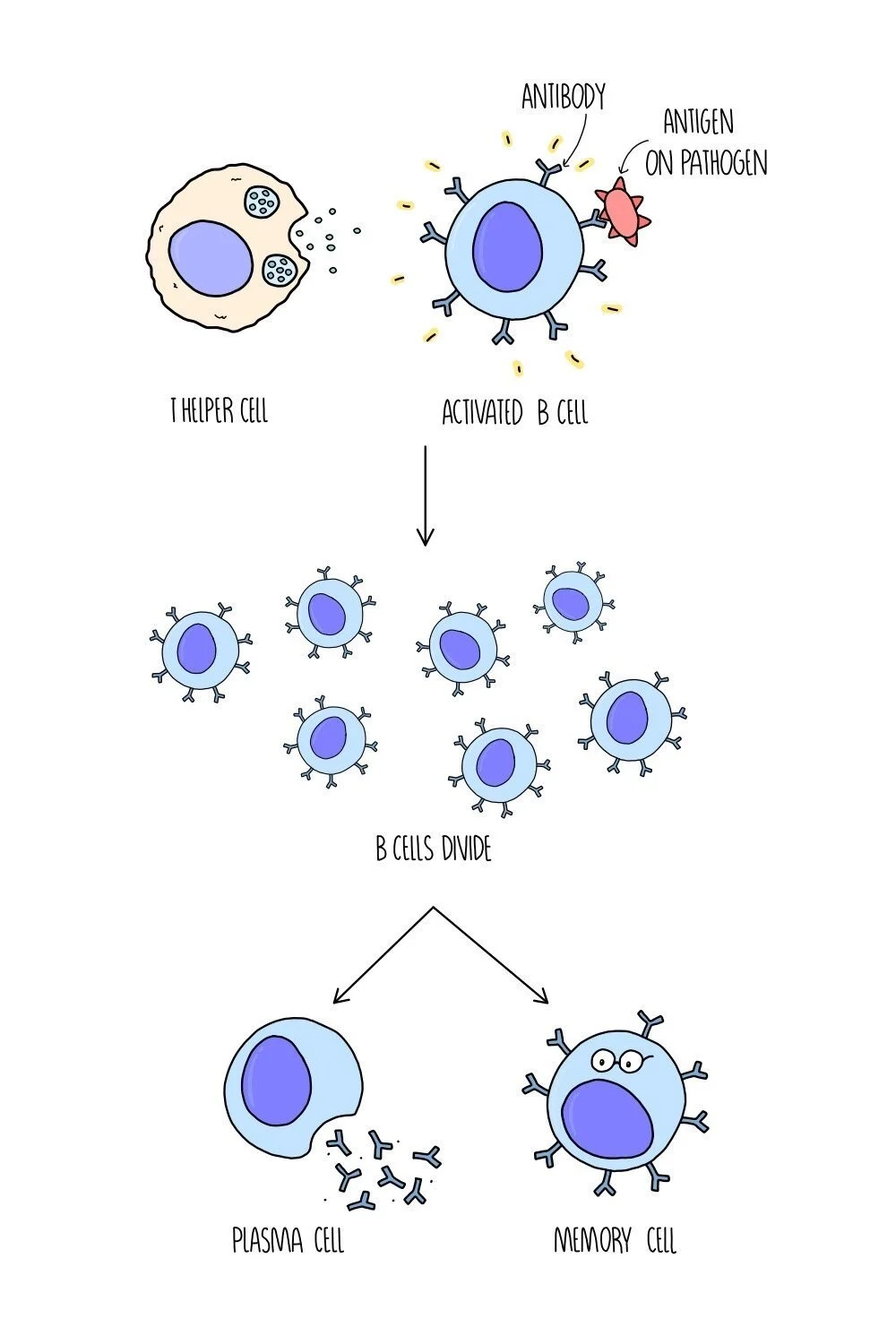
B lymphocyte response
B cells are activated when chemicals are released from T helper cells. They are also activated when the antibody molecules on their cell surface bind to a complementary antigen. Different B cells have different shaped antibodies on their surface, so only the B cells with the correct-shaped antibodies will be activated. Once they are activated, the B cells divide by mitosis and differentiate into two kinds of cell - plasma cells and memory cells.
Plasma cells produce antibodies with a complementary shape to the antigen.
Memory cells remain in the bloodstream in low levels in case reinfection occurs. If the antigen is detected again at a later date, they will quickly divide into plasma cells.
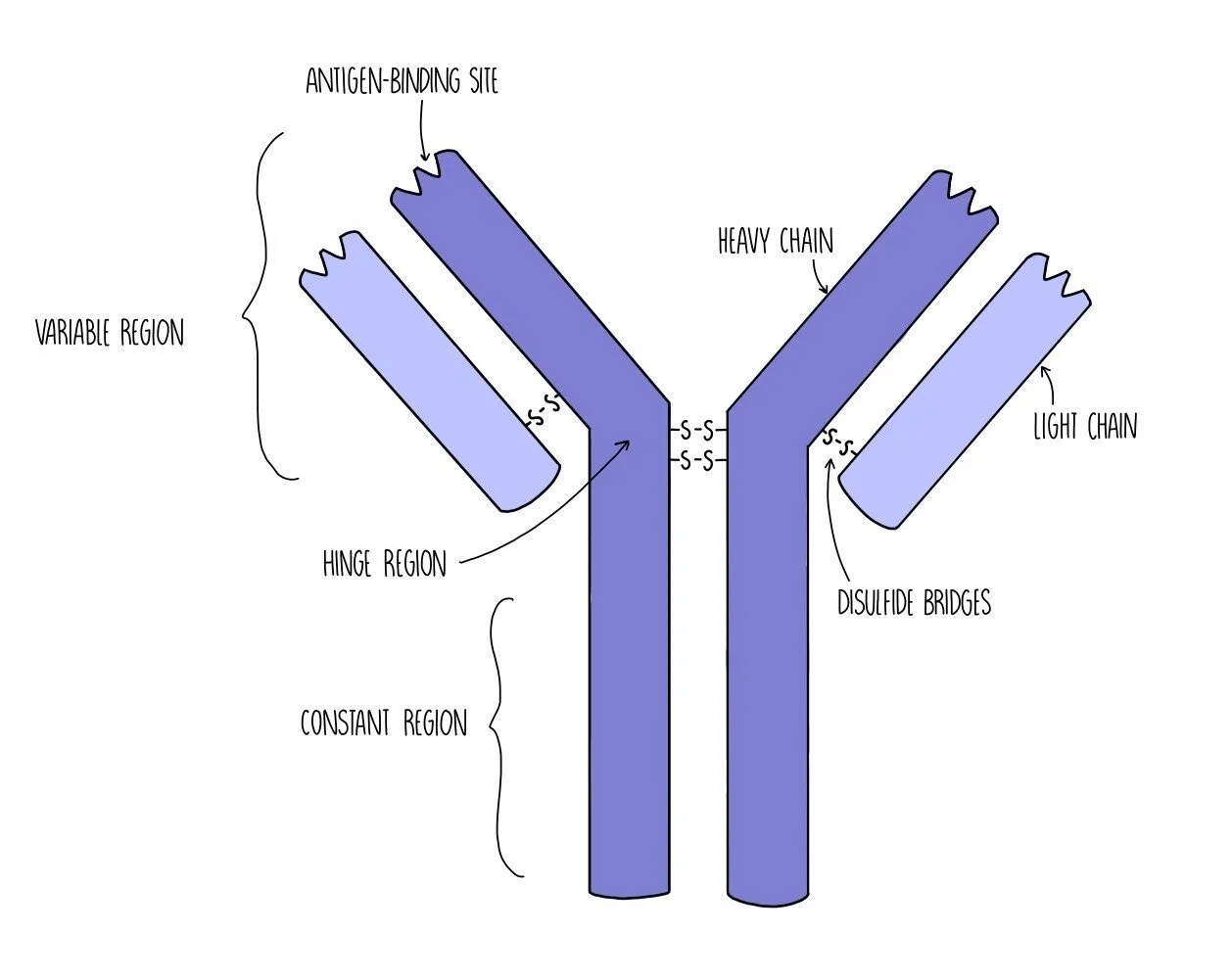
Antibody structure
Antibodies have a quaternary structure made up of four polypeptide chains (two heavy chains and two light chains) held together by disulfide bridges. They are composed of a variable region (which is different in different antibodies) where the antigen-binding site is located. The antigen-binding site has a complementary shape to the antigen which makes it specific to that particular antigen. There is also the constant region which is the same for all antibodies. The constant region contains another binding site which allows the antibody to bind to immune system cells, such as B cells or phagocytes. In between the variable region and the constant region is the hinge region which provides the antibody with flexibility.
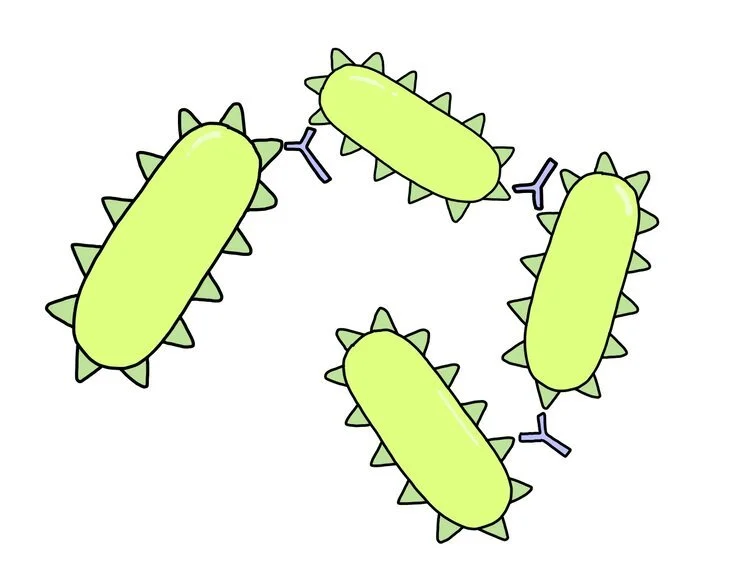
AGGLUTINATION OF PATHOGENS
How antibodies work
Antibodies work to destroy pathogens in three different ways.
Agglutination - antibodies each contain two antigen-binding sites which means they can bind to two pathogens at the same time. This causes pathogens to become clumped together. Phagocytes can then engulf and digest lots of pathogens at the same time, which makes phagocytosis more efficient.
Neutralising toxins - certain pathogens, such as bacteria, make us feel ill by releasing toxins. Antibodies can bind to toxins which renders them harmless (it neutralises them). The antibody-toxin complex can then be destroyed by phagocytes.
Blocking access to human cells - pathogens enter host cells when their antigens bind to receptor molecules on host cells (like a key opening a lock). When antibodies bind to antigens, it prevents the antigen from fitting in the receptor which means it can’t get inside the cell.
Cellular vs humoral immune response
The immune response can be split into two types of response which interact with each other:
Cellular immune response – includes phagocytosis and T-cell response
Humoral immune response – includes B-cells and the antibodies they produce
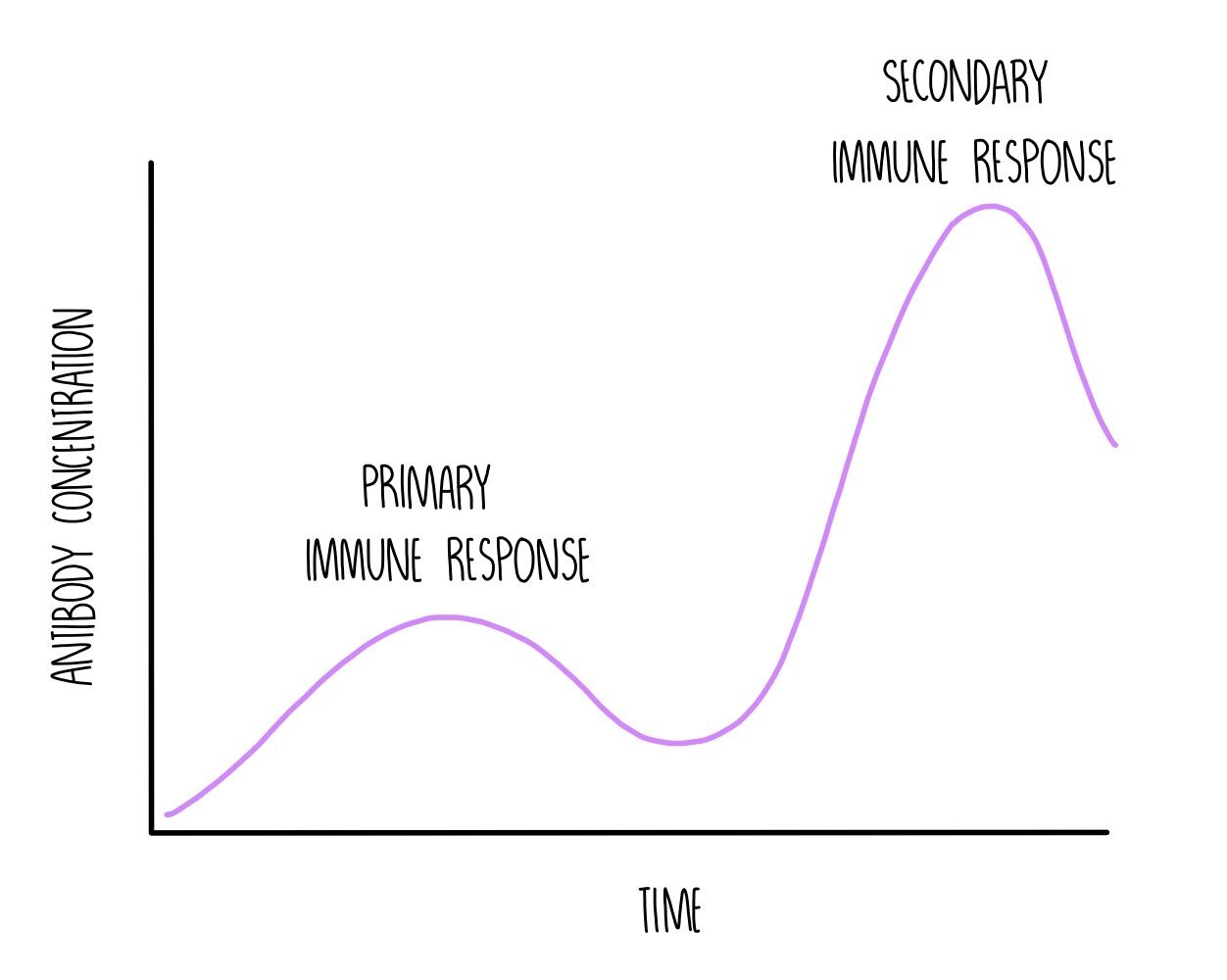
Primary and Secondary Immune Response
The primary immune response occurs when you are infected with a pathogen for the first time. It is composed of the non-specific and the specific immune response. This process is slow because it takes time for the correct B cell to be activated (clonal selection) and divide into lots of plasma cells (clonal expansion) in order to produce antibodies with a complementary shape to the antigen. The infected person will experience symptoms while the T and B cells mount an immune response. As part of the primary response, both T and B cells produce memory cells.
If you are re-infected with the same pathogen in the future, the T and B memory cells will recognise the antigen and start dividing. T memory cells will divide into the correct type of T killer cell to kill any cells that are infected with the pathogen. B memory cells will divide into plasma cells to produce a large number of antibodies which is complementary to the antigen molecules on the pathogen. This is the secondary immune response and is much quicker than the primary response. It happens so quickly that the pathogen is suppressed before you are able to experience symptoms - you are immune to the pathogen.
Vaccines
Vaccines contain a dead or weakened form of a pathogen which is injected into the bloodstream. Sometimes vaccines contain just the antigen proteins without the rest of the pathogen. Other vaccines might contain a variety of different antigens to protect against different strains of pathogens which vary in the shape of the proteins on their cell surface membranes (antigenic variation). The injection of weakened antigens stimulates a primary immune response and the production of memory T cells and memory B cells, resulting in immunity without becoming ill from the disease.
Antigenic variation
Pathogens are continually evolving to evade the immune system. One way in which they do this is by switching up the shape of their antigens, a process known as antigenic variation. Viruses like influenza and HIV have a high rate of mutation in the genes which code for its antigens. This means that different strains of the virus will show slight differences in the shape of their antigens. Memory cells that have formed from one viral strain may not detect the presence of antigens from other strains, so the person has to go through the primary immune response all over again. Antigenic variation makes it difficult to develop a vaccine for these pathogens and it’s why a new flu vaccine is released each year.
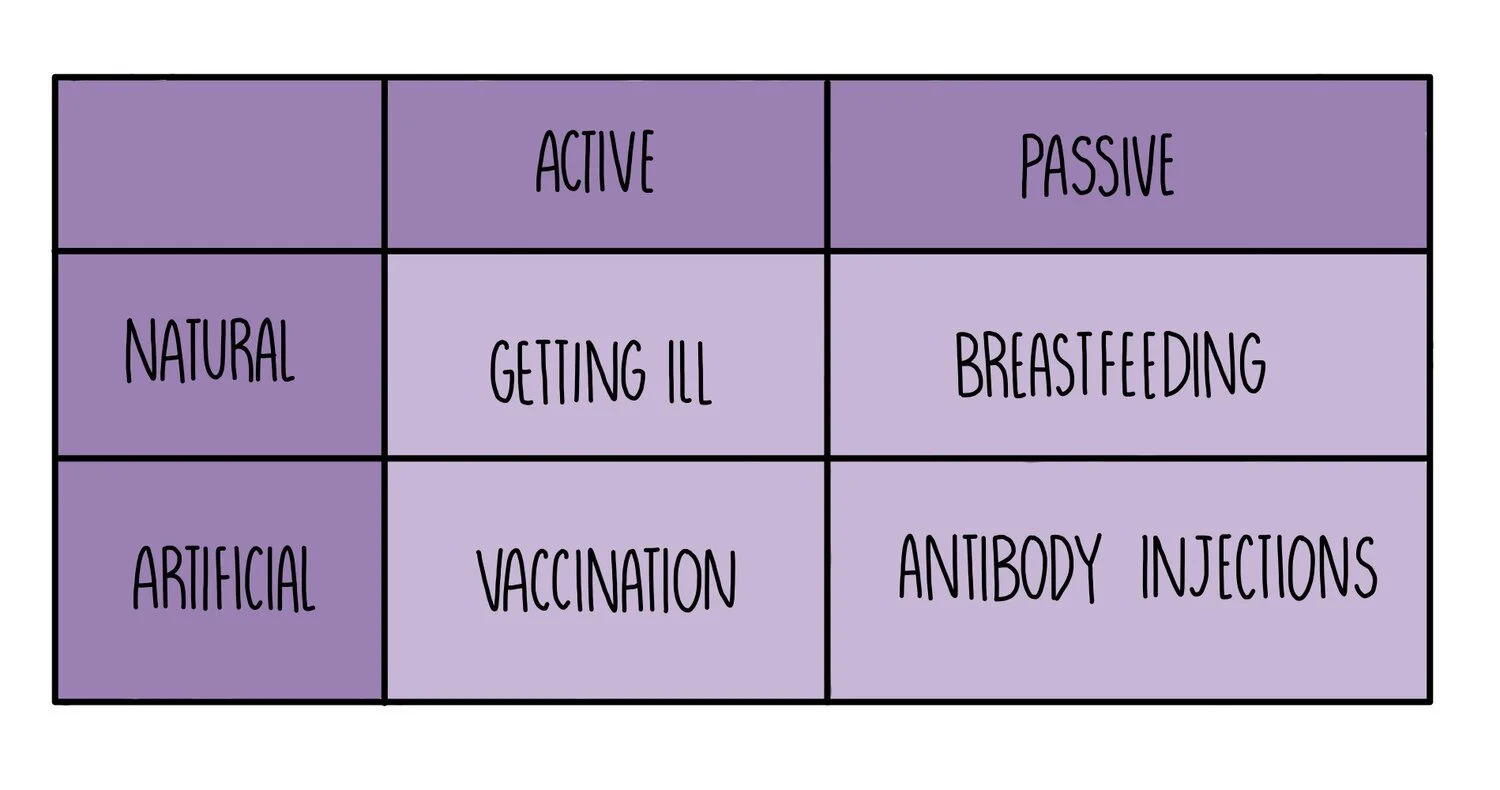
Active vs Passive Immunity
Active immunity occurs when your body makes its own antibodies after being stimulated by an antigen. This process can be natural (e.g. if you catch a cold, your body will make its own antibodies against the common cold virus) or it can be artificial (e.g. if you are vaccinated with a harmless form of an antigen).
Passive immunity occurs when you are given ready-made antibodies that have been produced by another organism. This process can be natural (e.g. babies receive antibodies from their mother when they breastfeed) or artificial (e.g. antibody injections can be given for some diseases - e.g. this is being tested as a treatment for Ebola).
Active immunity lasts longer since memory cells will remain in the body for years but it takes time to develop. Passive immunity provides immediate protection against pathogens but is short-lived (antibodies that are transferred from mother to child during breastfeeding only remain in the body for about 18 months).
Uses of monoclonal antibodies
Monoclonal antibodies are antibodies produced from a single B-cell clone so they all have the exact same structure. Monoclonal antibodies can be developed to bind to anything, not just antigens on a pathogen. For example, they can be engineered to bind to antigens on the surface of cancer cells to deliver a chemotherapy drug to the site of a tumour, minimising the impact on healthy cells. This works because tumour cells have different antigens compared to normal body cells.
Monoclonal antibodies are also used in pregnancy tests:
On the application area of pregnancy tests (the part that is urinated on), there are antibodies for human chorionic gonadotropin (hCG) hormone. The hCG hormone is released by foetuses, so is only found in the urine of pregnant women. The antibodies are bound to a blue bead.
If there is any hCG present in the urine, this will bind to the antibody on the beads.
The urine moves up the stick to the test strip, carrying the beads with it. The test strip contains immobilised hCG antibodies, fixed in position on the test strip
If hCG is present, the immobilised antibodies bind to the hormone that is already attached to the mobile hCG antibody and the blue bead. This causes the strip to turn blue, only if the hormone is present.
If hCG is absent, the beads pass through the test area without binding to anything so the test strip remains white.
ELISA test
The ELISA (enzyme-linked immunosorbent assay) test is used in medical diagnosis to see if someone has antibodies against a certain pathogen. There are two types: direct ELISA uses a single antibody that is complementary to the disease antigen. Indirect ELISA uses two different antibodies:
Antigens for a particular disease (e.g. HIV antigens) are bound to the surface of a dish.
A patient’s blood sample is added to the dish. If they possess complementary antibodies (e.g. HIV antibodies), these will bind to the antigens fixed on the bottom of the plate.
The blood sample is then washed off.
A solution containing secondary antibody is applied. These will bind to any HIV antibody that is bound to the plate. The secondary antibody is attached to an enzyme.
The solution is washed off to remove any unbound secondary antibody.
A substrate is added which will be converted into a coloured product if the enzyme is present. Since the enzyme is only present if the blood sample contained HIV antibodies, the colour change indicates a positive result for HIV infection. If the person does not possess HIV antibodies, no colour change will take place.
HIV and AIDS
Human immunodeficiency virus (HIV) is a deadly virus which can weaken a person’s immune system by destroying a type of immune cell called T helper cells. It is spread through the transmission of infected bodily fluids (e.g. during sexual intercourse, sharing of needles or blood transfusion). HIV doesn’t kill the patient directly, but weakens the immune system to an extent that the patient is unable to fight off other infections which normally would not pose a threat - these are known as opportunistic infections.
When the patient’s immune system has weakened to a particularly low level (this is seen by a low T helper cell count in hospital blood tests), the patient has developed a disease called acquired immunodeficiency syndrome (AIDS). The time between the initial infection and the onset of AIDS symptoms (the latency period) varies greatly between individuals but is usually around 10 years. The length of the latency period depends on the individual’s age, strength of their immune system and access to healthcare.
The symptoms of AIDS follow a series of stages:
The person will first develop less serious, minor infections which will gradually become more and more severe.
As the patient’s body tries to fight off more infections, the lower their T cell levels drop.
Eventually their immune system will be so weak that they will die of an opportunistic infection because they do not have enough immune cells to defend themselves.
HIV Replication
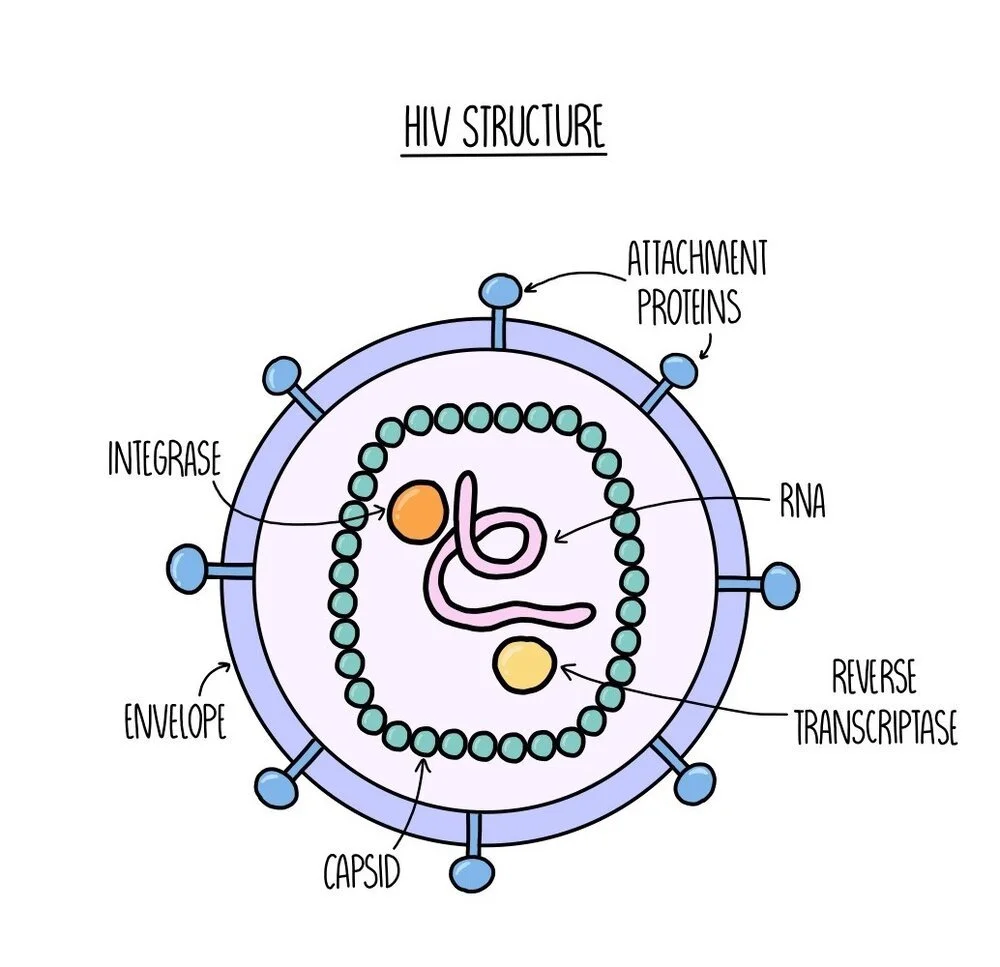
The HIV virus consists of a core of RNA and enzymes (reverse transcriptase and integrase) which is enclosed in a protein coat called a capsid. Surrounding the capsid is an outer layer called the envelope which contains attachment proteins - these proteins are crucial for the virus to enter host cells (they act like little keys to access our cells).
If a person with HIV exchanges bodily fluid with another person, HIV can infect the second individual and will be present in their bloodstream. The HIV virus uses its attachment proteins to enter human immune cells (specifically the T helper cell) by binding to receptors on the T cell. The capsid is released into the cell, where it breaks apart to release the RNA and enzymes. The enzyme reverse transcriptase converts the RNA into DNA. The single-stranded DNA is converted into double-stranded DNA which the enzyme integrase can insert into the DNA of the T cell. The T cell now has the ‘instructions’ (genes) to produce viral proteins. The viral DNA is transcribed and translated and the viral proteins are used to build new virus particles, which move out of the T cell and infect other cells.
Antibiotics
Antibiotics work by interfering with bacterial cell walls and ribosomes, either killing the bacteria or stopping its growth. They have no effect on viruses or our own cells because:
Viruses do not have ribosomes or cell walls, which means that antibiotic treatment is completely ineffective against viral infections
Human cells do not have cell walls. We do have ribosomes, but these are bigger than those found in bacteria and unaffected by antibiotics. This is useful, because it means we can take antibiotics without worrying about it interfering with our own cells.